What you will learn in this article:
- Symptoms of progesterone deficiency
- The role of progesterone in a woman’s body
- The benefits of topical progesterone
- Difference between synthetic and bioidentical progesterone
- What your progesterone should NOT contain
- The product I use and recommend
- What dosage and how to apply
This is Part 1 of the Progesterone Series. In Part 2, you will learn more about paradoxical cases and reactions to progesterone (rare but they happen) and what could be causing them.
You know I’m a big proponent of using food as the key tool to balance hormones. I would like to remind you that food is the foundation of your hormonal health.
Herbs and supplements can play a big role, too. My mantra on how to prioritize these modalities is simple:
If you are getting no results with diet and herbs alone, it might be time to explore bioidentical hormones, such as progesterone.
So who should resort to using topical hormones such as estradiol, estriol, DHEA or progesterone? It depends on the person. Don’t you just cringe hearing that? But don’t worry, I will break it down for you.
Some women can function beautifully without taking any supplemental hormones. Others might need progesterone only, and some might need all four of them. Furthermore, your body changes and over time you might see a need to increase some and decrease or drop others.
Most of the readers of Hormones Balance are women after age 45—it is therefore no surprise that many show signs of progesterone deficiency. In fact, ovarian production of estrogen can decline by as much as 60% and levels of progesterone can drop as much as 100% once ovulation ends. For some women that can happen as early as their 40’s.
Symptoms of Progesterone Deficiency
- Hot flashes and night sweats
- Insomnia and mid night waking
- Fertility or menstrual problems
- PMS or PMDD
- Anxiety and restlessness
- Irritability and nervousness
- Low mood and depression, especially around ovulation and pre-period
- Mood swings
- Weight gain and cellulite, especially around the thighs and buttocks
- Fluid retention – your fingers and toes swell up
- Brain fog
- Sagging skin
- Low thyroid
- Pain and inflammation
- Osteoporosis
- Excessive menstruation
- Hypersensitivity
- Migraine headaches before cycles
- Decreased libido
- Decreased HDL (“good” cholesterol)
The Role of Progesterone in a Woman’s Body
Progesterone is often mentioned as the hormone necessary in fertility and pregnancy but its role is far wider than that.
Here are some of the reported health benefits of having leveled progesterone levels—including women in peri- and menopause.
- Reduction of hot flashes and night sweats (this study shows a reduction as high as 80%)
- Improvement of bone health and osteoporosis—even osteoporosis (by having an osteoblastic effect)
- Reduction in PMS symptoms, bloating, water retention, and mood swings
- Restoration of a healthy menstrual cycle (less bleeding, shorter days)
- Restoration of ovulation and a healthy luteal phase (women in peri-menopause often experience shortened luteal phase)
- Improve quality of sleep
- Reduction of uterine fibroids and endometriosis
- Reduction of pelvic pain
- Improved libido
- Increased thyroid function (shown to increase free thyroxine)
- Breast cancer prevention (studies here and here)
- Improved fertility, ovulation and health of the first-trimester pregnancy
- Reduction or disappearance of breast lumps
- Progesterone inhibits mast cells releasing histamine
- Relief of pain in fibrocystic breasts
- Deeper and more restful sleep
- Mood enhancement
- Anxiety relief
- Anti-inflammatory effect—I used it post-surgery as well to lower the inflammation
- Potential support with autoimmune and inflammatory diseases
- Improved brain health
- Supports recovery from TBI (Traumatic Brain Injury)
Progesterone and Estrogen Dominance
Low progesterone symptoms result not just because the body needs progesterone to stave off these symptoms but also because of the impact of the progesterone to estrogen ratio.
When progesterone levels drop below a certain level, estrogen becomes the dominant hormone, and this change in the balance between the levels of these two hormones is what ultimately leads to many of the symptoms that people experience when their progesterone levels go down.
When this imbalance occurs, certain herbs can help to restore balance, but sometimes progesterone is needed to relieve problematic symptoms.
Why Can Women Get So Depleted in Progesterone?
Several factors make it more likely for your progesterone levels to drop.
The 3 primary factors are:
Age
As you get older, your estrogen and progesterone levels both drop. However, because progesterone drops more significantly, the estrogen to progesterone ratio becomes higher than it was when you were younger, which is associated with estrogen dominance symptoms.
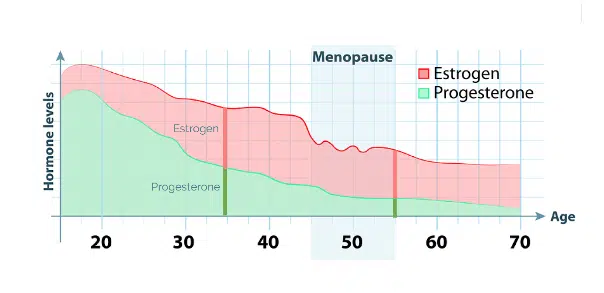
Take a look at the chart below—it shows the drop of estrogen and progesterone over time. Can you see how, for example, a woman age 35 has her estrogen and progesterone at about 1:1 ratio? Now take a look at how that changes when she is 55: her estrogen, even though it’s lower, it’s more dominant as compared to her progesterone levels.
This imbalance may also account for why older women are more likely to develop estrogen receptor-positive breast cancer at the later age—the culprit is estrogen dominance with low progesterone levels.
Stress
Stress can cause progesterone levels to drop. When we are stressed, we produce and release higher levels of the hormone cortisol. Both cortisol and progesterone are produced from pregnenolone. When you are in chronic stress, the body will prioritize and divert the available pregnenolone to produce higher amounts of cortisol to help you get through stress.
This means there might not be enough to produce sufficient levels of progesterone. This is called “pregnenolone steal” and it’s the leading cause of low progesterone problems.
Toxic Skincare and House Cleaning Products
The use of toxic cosmetic products or house cleaning products introduce molecules known as xenoestrogens, which interfere with normal female sexual hormone activity. Using these types of products can cause imbalances in the estrogen to progesterone ratio and thereby lead to symptoms associated with low progesterone.
Other causes can be:
- Antidepressants
- Excessive arginine consumption (often used in heart and blood vessel conditions including congestive heart failure (CHF), chest pain, high blood pressure, and coronary artery disease)
- High sugar consumption, high blood sugar levels
- Consumption of trans fats
- Deficiency of vitamins A, B6, C and zinc
The Benefits of Topical Progesterone
At the beginning of the article, I mentioned how food, nutrients, and herbal solutions can naturally boost progesterone levels.
However, there might be circumstances where you can’t or won’t change your diet or have no access to these herbs. Or perhaps, which I hope is not the case, you have tried nutritional strategies but are still highly symptomatic. In these circumstances, topical progesterone might be a good solution.
This is when I brought on topical progesterone and felt instant relief. I also felt much calmer during the day, in spite of the barrage of challenges.
Therefore, in times of acute stress, such as divorce, work deadlines, or illness, bringing in topical progesterone might be a great idea.
Topical or Oral Form of Progesterone?
Putting topical progesterone on your body allows it to bypass digestion and the liver which is good for two reasons.
One, you don’t tax your digestion and liver with yet another compound to be absorbed and metabolized.
Two, if your gut and liver aren’t functioning optimally, you are running the risk of your body breaking down progesterone into “dirty” progesterone metabolites, which can be harmful.
Furthermore, oral progesterone is largely converted to allopregnanolone on its first pass through the liver. This isn’t the best choice as a progesterone replacement therapy because allopregnanolone attaches to GABA receptors, creating anxiolytic (anti-anxiety) and somniferous (induces sleep) effects. Oral progesterone does not offer all the other benefits of progesterone (described above).
For these reasons, I recommend progesterone in a topical form, not an oral form.
The Difference Between Bioidentical and Synthetic Progesterone (Progestin)
Until today, there is fear among women and misinformed doctors of using any form of hormone replacement therapy (more on that below). This fear can be debunked once we understand that there is a big difference between bioidentical progesterone and progestin.
True progesterone is naturally produced by the body.
Progestins (brand names include Prempro) come from pregnant mares and are synthetically altered in laboratories. The problem with progestins is that they don’t “fit” into the progesterone receptor the way natural progesterone does—their molecular structure is different which can cause a host of health issues (more on that below).
They are referred to HRT which stands for “Hormone Replacement Therapy.” Progestins are also used in birth control pills and often presented by doctors as “safer” than estrogen-based contraceptives, which is misleading and incorrect.
The side effects from using progestins can include:
- Increases appetite
- Weight gain
- Fluid retention
- Irritability
- Depression
- Headache
- Decreases energy
- Bloating
- Breast tenderness
- Decreases sexual interest
- Acne
- Hair loss
- Nausea
- Insomnia
- Interferes with the body’s own production of progesterone
- Does not help balance estrogen
- Remains in the body longer
Bioidentical progesterone, also called “natural”, is derived from plants—typically from yams or soy. To be clear: they are also created in a lab but the molecular structure resembles true progesterone produced by your own body.
Yam or soy in their natural form whether eaten or applied topically, will not have the same effect as bioidentical hormones. If you watched the TV series “Frankie and Grace,” Frankie starts a new business venture making yam cream from her boyfriend’s harvest to boost progesterone in women. It’s a cute and funny story but it’s also misleading. Women who report improvement on yam creams are probably experiencing the placebo effect.
“Progestogen” (sometimes spelled “progestagen”) is a general term for hormones that act like progesterone, and therefore includes both progesterone and progestins. That’s what California Prop 65 warning contains. It covers “Progestogen” and the warning is based on the use of progestins and NOT progesterone.
Effects from Bioidentical Progesterone Not Seen with Progestins
I want to address one vital issue: Not all hormones are the same. So many women are terrified by them, are told by their misinformed physicians in a blanket statement that “hormones cause cancer.” As a result, women go through life suffering from an awful load of symptoms that would be resolved by using bioidentical hormones.
I recently attended an endocrine symposium and learned even more about progestin and what they DO NOT help do (while natural can help with all these):
- Helps balance estrogen
- Leaves the body quickly
- Improves sleep
- Natural calming effect
- Lowers high blood pressure
- Helps the body use and eliminate fats
- Lowers cholesterol
- Increases scalp hair
- Helps balance fluids in the cells
- Increases the beneficial effects of estrogen on BV
- Increases metabolic rate
- Natural diuretic
- Natural antidepressant
- Is anti-inflammatory
- Stimulates the production of new bone
- Enhances the action of thyroid hormones
- Improves libido
- Helps restore proper cell oxygen levels
- Induces conversion of E1 to the inactive E1S form
- Promotes Th2 immunity
- Is neuroprotective, promoting myelination
As you can see from this long list, natural progesterone and progestin might as well be called two completely different chemicals.
Furthermore, studies (here and here) have shown that progesterone does NOT induce estrogen-stimulated breast cell proliferation.
Does Hormone Replacement Therapy Cause Cancer?
The scare of hormones causing cancer and other health issues started with the World Health Initiative. It studied more than 15,000 women between the ages of 50 and 79 who were given HRT in the form of estrogen and progestin (not bioidentical progesterone) for a period of over 10 years.
The study had to be stopped early due to the high occurrence of breast cancers, blood clots, strokes, and cardiovascular diseases. This sent waves of fear amongst women and doctors and all hormones were declared unsafe. Many doctors have never been educated and updated on the nuance of this study and issue a blanket statement to their patients, which doesn’t serve women, especially those who need it badly.
Enough studies have been done to date to establish, over extended periods of time, that bioidentical progesterone is a completely different compound and its benefits outweigh the risks.
For example, this study demonstrated that progestin and norethisterone (a synthetic and potent progestogen hormone used to stop uterine bleeding) caused the proliferation of progesterone receptor breast cancer cells.
This study compared bioidentical estrogen and progesterone to horse-derived estrogen and progestin, and concluded: “By contrast, two 28-day cycles of daily oral conjugated equine estrogens (CEE) 0.625 mg and oral medroxyprogesterone acetate (MPA) 5 mg for the last 14 days of each cycle significantly increased proliferation at both the cell level and at the mRNA level, and significantly enhanced mammographic breast density, an important risk factor for breast cancer.”
This study has demonstrated that the “Exposure to progesterone for 14 days reduced the estradiol-induced proliferation of normal breast epithelial cells in vivo.” This is important because carcinoma is a malignancy of the epithelial tissue and it accounts for 80 to 90 percent of all cancer cases.
One more study I want to share with you found that natural progesterone has been shown to decrease the risk of developing breast cancer. This study looked at 80,000 postmenopausal women for 8 years using different forms of HRT. It found that women who used estrogen in combination with synthetic progestin had a 69% increased risk of developing breast cancer when compared to women who never took HRT. Women who used progesterone in combination with estrogen had no increased risk in developing breast cancer compared to women that did not use HRT and also had a decreased risk in developing breast cancer compared to the women that used progestin.
Can Progesterone Be Used for Cancer Prevention?
Yes. Most of my colleagues who practice functional medicine and specialize in women’s health prescribe progesterone as a way to prevent estrogenic cancers such as breast, ovarian and uterine cancers. Progesterone protects against endometrial and breast cancer. The 1981 Johns Hopkins study found that infertile women with progesterone deficiency had a premenopausal breast cancer risk that was 540% greater than that of women whose infertility was not related to their hormone status. Furthermore, these women had a 1,000% greater risk of death from all types of cancer. Studies showed that progesterone suppressed the cells from spreading and induced cell death in malignant mesothelioma cancer cells and that it also can inhibit growth and cause cell death in breast cancer cells.
How to Choose Your Topical Progesterone
If you are ready to give it a try, here are a few guidelines on what bioidentical progesterone should NEVER contain:
- Parabens (a form of xeno-estrogens that mimic estrogens)
- Mineral oil
- Petroleum
- Fragrance (they contain phthalates which are toxic estrogens)
- Yams in their direct form (they are not harmful, just ineffective and you are wasting money)
What I Use and Recommend
Because of my personal experience of using topical progesterone (in the past and present—as I’m going into perimenopause at age 46), I turned to one of the top experts in the country to help formulate our own Wellena topical progesterone: ProgestPure Cream.
ProgestPure Cream is a natural topical progesterone cream providing 25 mg of bioidentical progesterone in every serving (of 4 pumps). This highly bioavailable progesterone cream is very clean, contains a gentle preservative system, and is free of parabens, mineral oil, and petroleum.
Where to Apply Topical Progesterone and Why
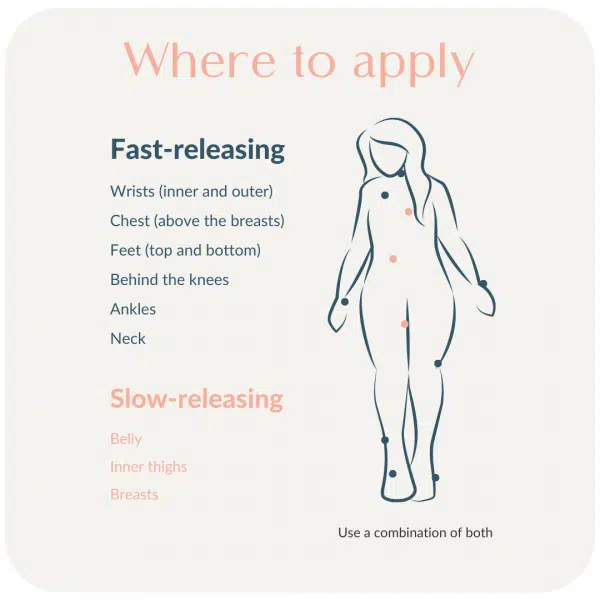
Rotate where you apply the topical progesterone, and in doing so, switch between fatty and non-fatty areas. Whereas fat will store the progesterone and absorb the progesterone into capillary blood, progesterone applied to thinner areas will more readily be taken up into the body and metabolized.
Uptake is best in the places where you blush—such as the face, neck, and chest. Rotating whether progesterone is put on fat or thin areas of the body can help to produce both immediate and sustained benefits of topical progesterone.
When to Use Topical Progesterone?
Women finished with menstruation (or nearly finished with menstruation)
Women going through peri-menopause, menopause, and post-menopause; who suffer from sleep disruption, hot flashes, or night sweats, can use topical progesterone for up to 25 days out of a 30-day calendar, with 5-7 days off, or as recommended by your healthcare provider.
Menstruating women
Menstruating women are advised to use topical progesterone 5 to 7 days after the first day of your period and continue until the next period begins. Day 1 is the first day of your menstrual bleed. If your period is irregular, start using topical progesterone 7 days after you begin a period and teach your body to learn a new cycle. Stop whenever your period comes back again, and repeat, or apply as recommended by your healthcare provider.
Women with no ovulation like in the case of PCOS can pick a day and start 7 days after the first day of the period and continue until the period starts again.
How Much Progesterone Should You Use?
It will depend on how low and symptomatic you are, your diet, and stress levels (remember the pregnenolone steal I talked about above?). I recommend starting slow and then dose up.
If you choose to use ProgestPure Cream, start with four pumps which will give you 25 mg of bioidentical progesterone. You can double that (by doing it twice a day) to 50 mg per day if symptoms don’t improve.
Another way to dose is to use your body weight.
Women under 150 lbs: start with 20–30mg of bioidentical progesterone.
Women over 150 lbs: start with 40-50mg of bioidentical progesterone.
If you want to try a higher dosage, I recommend working with a skilled functional practitioner who knows the ins and outs of bioidentical hormones and tests your levels to be sure that you don’t overproduce the “dirty” progesterone.
Will I Start Feeling Worse Before Feeling Better?
It can happen. I suggest reading more on paradoxical reactions to progesterone in Part 2 of the Progesterone Series. Some women experience exacerbated symptoms of estrogen dominance (such as tender breasts and poor sleep) before they feel better. Functional practitioners recommend reducing the dose by half (meaning: 10mg per day) and trying that for a month before slowly titrating up. If you find no relief, I recommend working with a skilled practitioner who can guide you. If you need help finding one, please email my team here and we will do our best to help.
Who Should NOT Use Progesterone?
Women with progesterone receptor-positive breast cancer should not use topical progesterone, even though progesterone is likely not the main culprit in this form of breast cancer.
According to functional oncologists and functional endocrinologists, the problem is in how the body breaks down progesterone into specific metabolites (I call them “dirty” progesterones) that can cause problems, as well as the use of progestins like those in birth control pills. Furthermore, as also mentioned above, the use of synthetic estrogen and progestin is a likely culprit behind ER+ and PR+ breast cancers.
Furthermore, research has shown that the use of birth control pills could increase the risk of breast cancer and may contribute to a substantial number of breast cancer diagnoses. Nevertheless, until there is more research to more clearly elucidate the causes and contributing factors associated with progesterone receptor-positive breast cancer, I do not advise the use of topical progesterone for these individuals.
In addition to the breast cancer patients described above, those with hormonal issues, and those receiving doctor’s advice not to use it should not use topical progesterone.
In Part 2 of the Progesterone Series, I will talk about the paradoxical responses to progesterone (rare but they can happen).
Disclaimer
These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease

Cannot Download Supplement Guide for hormonal balance. Would it possible to have it emailed to me?
Thanks
Hi Nancy, sure! Please email Magdalena’s team at [email protected] and we will be happy to email you the guide. ~ Jeanne HB Team
Is it possible to ship to Norway? If not, do you reccomend an other brand from Iherb or Amazone that ship?
Hi Nancy, Unfortunately, we are not shipping internationally at this time due to the difficulties with supplements going through customs. If this changes, we will send out an update regarding this policy. Thank you for understanding.
Magdalena has only researched and used this progesterone, but you might want to check to see if Designs for Health sells Progest-Avail internationally on Amazon.
I hope this helps!
Jeanne HB Team
Hi, I live in Central Florida. Would you send me a list of functional practitioners please? I am currently on bio-identical hormones but I think I am over-medicated – I am still fatigued and am developing skin tags. Thank you so much.
HI Rebecca, Here is a good tool to locate a functional medical practitioner in your area: https://www.functionalmedicine.org/practitioner_search.aspx?id=117
I hope this helps!
~Jeanne HB Team
Thank you for your article! I have been taking Activella for about 20years and feel great! But of course I certainly don’t want to be at risk for a stroke or cancer. I would like to have my hormones tested and then I would like to start the pure product right away! Is estrogen needed as well?
Is your progesterone good for me cause I had a hysterectomy??
Hi Hattie,
Yes, in fact, it should even though most conventional doctors only prescribe estrogen. Functional endocrinology recommends for women with full or partial hysterectomy to supplement with both estrogen and progesterone. ~Deanna HB Team
My practitioner put me on progesterone and it didn’t help with my sleep or periods and my breast grew one bra size. Do you know why this would happen?
Hello,
I am anxious to know about part 2. I experienced early menopause at maybe age 40 when my cycle stopped. By age 44 I found a naturopath and she put me on both topical cream based bioidentical hormones because I was low on both, but when I start on progesterone I experience similar side effects. A higher dose made me super sleepy. When I start dosing my breast plump up, and my liver feels inflamed, more hair loss and sever ill mood. It makes me angry. It is unfair to my loved ones. This is so contrary to everything I have read that I am so frustrated with myself. I don’t get why this is occurring is there any recommendations for me.
Lorena
Progesterone makes estrogen receptor sites more sensitive. You may have been estrogen dominant due to meat/dairy/soy/BPA/chemicals/fat/The Pill/flax/baby formula etc..
Hi Heather, which form of progesterone did your doctor put you on? If it wasn’t bioidentical that could be the reason. We always suggest you work with a practitioner who specializes in bioidenticals and recommend the DUTCH test to determine hormone imbalances.
~Jeanne HB Team
They told me it was Bioidentical
Hi Heather,
There may be side effects as with any medication or hormone therapy. Estrogen side-effects may occur when progesterone therapy is initiated. Estrogen symptoms such as headaches, nausea, depression and others sometime get worse with progesterone replacement, particularly when the dose is small. Progesterone stimulates estrogen receptors for estrogen. The initial stimulation occurs and potentiates the estrogen effect. When activity is potentiated, the amount of non-converted progesterone may not be enough to counter or balance these symptoms. Higher doses of progesterone may be needed or it may not be a fit. It is good to discuss this with your practitioner and possible try a different route of taking it. ~Deanna HB Team
Hello ! do you ship to Greece ? I’m very interested. thank you
Hi Jacquelina,
Unfortunately, we are not shipping internationally at this time due to the difficulties with supplements going through customs. If this changes, we will send out an update regarding this policy. Thank you for understanding.
It is suggested you follow the guidelines Magdalena mentions in this article when looking online or in your area- no parabens, fragrances, mineral oil…I hope that helps.
Great info! Can you take too much Progesterone and would weight gain be a side effect?
Hi Julie, we recommend working with a practitioner who specializes in bio-identical hormones and the Dutch test to determine if you need progesterone.
If you would like help finding a practitioner in your area, here is a helpful tool: https://www.functionalmedicine.org/practitioner_search.aspx?id=117.
Jeanne HB Team
Progesterone helps the thyroid and gets rid of water weight, but going too high may not be good.
Hi, can someone explain please why menstruating women should start progesterone 2 weeks before period day 14 and not on day 7. Would starting earlier do any harm?
Hi Olya,
Naturally progesterone levels are usually low during the first stage (follicular stage) of your menstrual cycle. Ovulation is called the luteal stage, when the egg is released into the fallopian tube. After ovulation (around day 14), progesterone levels go up for about 5 days before going back down. Progesterone prepares the endometrium to receive and nourish a fertilized egg. If pregnancy does not occur, progesterone levels decrease. The decrease in progesterone triggers menstruation, or shedding of the lining. If you started progesterone early, you could be altering this natural hormonal process. A quick google search of a progesterone/estrogen graph of menstruating women will bring up a good visual to help understand this reproductive process. =)
I hope this helps!
Healthy Regards,
HB Team
Hi Hattie, please consult your doctor or work with a bioidentical specialist to support you with bioidentical hormones.
~ Jeanne HB Team
Do you have part 2 available? I am interested in dirty progesterone. Had testing done by my functional medical doctor and my progesterone was 160,000 which she said she had never seen anyone so high. My estrogen was dropping and my
DHEA was normal but my testosterone was very high. I had been taking Natpro biodentical progesterone ( same ingredients as yours) for a few months( about 400-600 mg per day) to help with sleep and also supplementing with pregnenone for awhile. It didn’t help much with sleep. I was recommended to go off the progesterone in May and get retested. Now i notice i am getting hot flashes on a regular basis . Can you speak about dirty progesterone and negative side effects and also recommend a test that is cheaper than the Dutch. I don’t have the money for it now. Last time i tested with Genova and it was $300
Genova was $450 for me I think. They are a great company. Taking bioidentical hormones may shut down glands. MACA (cooked/gelatin) may nourish glands and stop hot flashes. NO gluten/dairy/soy/sugar/GMO/food with a label/heated oils..taking vitamins/good oils/minerals…probiotic…LDN..detoxing help me. Starting test for hormones may help, but going by symptoms after that worked for me. DHEA helps make hormones. My hormones had shut down. Your glands/hormones are still working/being made by DHEA?
Greetings, Can it be shipped to New Zealand, also can be recommended for people who suffer from PCOS? Thanks
Hi Sanji, Unfortunately, we are not shipping internationally at this time due to the difficulties with supplements going through customs. If this changes, we will send out an update regarding this policy. Thank you for understanding.
Please follow the guidelines in the article Magdalena wrote on how to choose a topical progesterone cream.
We advocate balancing your hormones in this order of priorities:
Dial in your diet (anti-inflammatory foods, good gut health, healthy liver, and stable sugar levels).
Add natural tools such as the seed rotation.
Only then, add the supplements.
If that’s not enough, consider bioidentical hormones. Bioidentical hormones are not the same as hormone replacement therapy (HRT) of the 90’s. There is very good supportive evidence of how they can work for us.
If you want to learn about how food can balance hormones, here is our workshop https://hormonesbalance.com/cfb.
And, here is a little quiz to give you an idea of possible hormonal imbalances https://hormonesbalance.com/quiz/.
I hope this helps!
Jeanne HB Team
Hiya – I’m from NZ and I was able to buy some of Magdalena’s products. How you do it is set up an account in You Shop on the NZ Post website. They will send you your USA shipping address. That’s what you put into the Hormones Balance website. Then You Shop will contact you when the item has arrived at the USA warehouse. Then you pay You Shop to ship it to NZ. Very easy to do!
Thank you for sharing this method of international shipping Sasha 🙂 ~HB Team
Hello! I’m wondering if this can be helpful for women who have lost their cycles due to stress?
I’ve done a revamp in my stress management, removed inflammatory foods, and added supplements recommended by a naturopath, but still no cycle in sight.
I have tested my blood and I have low free T3, low estradiol, and low progesterone.
Based on the limited information here, can you recommend topical progestrone?
Hi Taylor,
It is something that can be tried. The body has an amazing capacity to heal. ~Deanna HB Team
Yes…stress uses up B vitamins/Zn/progesterone. No gluten may help the thyroid/glands. MACA (cooked/gelatin) may nourish glands.
Hi Taylor, We advise you speak to a skilled practitioner who specializes in bioidentical hormones to determine if this is something you need. Magdalena released the second article about progesterone today that you might find helpful. Here is the link: https://hormonesbalance.com/articles/topical-progesterone-when-why-and-how-part-2
I hope this helps!
Jeanne HB Team
Hi,
You mention to take progest pure on days 14-28. Are you recommending stopping on day 28, regardless of whether or not you’ve starting bleeding? Sometimes I’m regular at 28 days but sometimes I may bleed on day 30 or 31. Should I stop at Day 28 regardless or wait for bleeding to begin before stopping? Is it possible to suppress the start date of bleeding/menstruation due to take the progest pure? (I ask because I’ve been taking and am on day 30 with no bleeding happening, and negative pregnancy test so I know it’s not that 🙂
Hi Sara, Correct: “For menstruating women it is advised to use topical progesterone during their luteal phase, which is day 14 to 28 of your cycle. Day 1 is the first day of your period. If your period is irregular, start progesterone on day 14 nevertheless.” ~ Jeanne HB Team
So, I’m still a bit confused. I thought average menstruation cycles begin on day 28, therefore isn’t it technically day 14-27 that we apply the progesterone oil? Or are you saying that we apply it on the first day we start menstruating, as well?
Secondly, I’ve been researching the comment above regarding fat storage (Dr Mercola site: “Progesterone cream must be used cautiously when applied to skin as progesterone is highly fat soluble and will accumulate in fat tissue, thereby disrupting adrenal hormones such as DHEA, cortisol, and testosterone”)… I believe I may be suffering from this issue after using Progesterone in the past and applying it to thigh area (as suggested by my functional doc). I have gained weight that I can’t shake off and my cortisol is way off… Can Magdalena please look into this, and see if applying on the labia is optimal? I don’t want to purchase, and then cause more harm.
Lastly, I’m not sure as to where she says to place on the body (face – where and how many drops exactly)? What is an example of rotating (ie 10 drops face, 5 drops neck, 5 drops labia etc). Would be great if she could be a bit more prescriptive on how exactly to apply. TY
Hi Dee,
Menstruation is day 1 of a cycle. You apply progesterone from day 14 if still cycling regularly or day 7 if in peri-menopause, not planning to have kids and still symptomatic with symptoms such as hot flashes. Many practitioners prescribe applying in the thin layers of skin like the inner wrist while others recommend to rotate between thin and fatty tissue. I can’t imagine that applying Pg to fatty tissue would cause such hormonal disregulations. Finally, our ProgestPure wasn’t designed to be applied to the labia or vulva.
Healthy Regards, HB Team
If you have a short luteal phase, and then finally get pregnant, should you stop using it?
Hi Rose,
I would discuss this with my doctor to know what best for you and baby. Wish you the best!
Healthy Regards,
HB Team
Hi Sara,
My doctor advised me to take Utrogestan on days 14-26, if I expect the bleeding to start on day 28. Maybe that`s different with creams and oils.
Good luck!
Rosa
Hi, there is information out there now suggesting that putting it on the skin leads to fat stores that can cause health issues in the future and take up to 2 years to clear up; I’ve read on a few sites including Dr Mercola’s that it’s better to apply to the labia so that the hormones go through as close to where nature intended as possible, what’s your thoughts on this? I am estrogen dominant partly due to full hysterectomy and being on estradot. I’ve cut my patch down now to 12.5mcg and was put on utrogestin caplets but I’m pretty sure I’m not getting enough progesterin from them due to the way the liver processes it since I’m still having major sleep issues and palpitations and digestive issues too. Since I’m in NZ I can’t purchase your product so I”m trying Ona’s instead since they can ship to me.
Hi Rachelle, Here is where Magdalena suggests in the article to apply the progesterone:
Where to apply topical progesterone and why?
Rotate where you apply the topical progesterone, and in doing so, switch between fatty and non-fatty areas. Whereas fat will store the progesterone and absorb the progesterone into capillary blood, progesterone applied to thinner areas will more readily be taken up into the body and metabolized.
Uptake is best in the places where you blush – such as the face, neck, and chest. Rotating whether progesterone is put on fat or thin areas of the body can help to produce both immediate and sustained benefits of the topical progesterone.
Please work with a practitioner who specializes in bio-identical hormones. If you need help finding someone in your area here is a helpful tool: https://www.functionalmedicine.org/practitioner_search.aspx?id=117.
~Jeanne HB Team
Hi Rachelle,
Since you are in NZ, you may want to consult with Lara Briden or Kate Powe, who are naturopathic doctors specializing in women`s health or read their blogs.
Good luck!
Rosa
People can experiment on skin sites, but they suggest you rotate sites. Progesterone may help sleep/help thyroid/lower swelling/inflammation. Gluten may hurt the gut lining/glands/lower hormones etc. Low oxygen in the brain may cause sleep issues. Tiny amount of Himalayan salt before bed helps me sleep. Each person is different. I need all three hormones…estriol/progesterone/testosterone. Fat makes estrogen/gluten may lower the thyroid. Genova test for hormones/hair test for good mineral/heavy metals and more help me.
The article says to start with 20mg (milligram) of Progesterone. The typical amount of progesterone in the body is 5-20ng/ml (nanogram). 20 mg is 20,000,000ng of progesterone. This seems far too high for biological levels.
Hi Exi, Thank you for sharing your feedback. We always suggest working with a practitioner who specializes in bio-identical hormones. If you need help finding someone in your area, here is a heplful tool: https://www.functionalmedicine.org/practitioner_search.aspx?id=117.
~ Jeanne HB Team
20 mg as this article states is actually a very low dose. A lot of ladies such as I are actually in the range of 150-300 mg of bio identical progesterone. I don’t quite understand your calculations. I recommend you see a naturopath who specializes in bio identical hormones for correct info on dosing according to your body’s needs.
May I use progesterone cream while i am breastfeedind? I have a toddler one (2 years).
Hi Amanda, we are unable to advise on this for liability reasons. We always suggest working with a practitioner who specializes in bio-identical hormones. If you need help finding someone in your area, here is a heplful tool: https://www.functionalmedicine.org/practitioner_search.aspx?id=117.
~ Jeanne HB Team
Hormones may shut down glands if glands are not used. Progesterone may start ovulation and you would get pregnant maybe. I had a hard time starting hormones before my regular hormones were still cycling. It is much better to wait until menopause for hormones. A person can avoid soy and others making them estrogen dominant….(meat/dairy/soy/BPA/chemicals/own fat/The Pill/flax etc. My progesterone may have been low for a long time before I started the Bioidentical hormones due to gluten/burning out my adrenals from stress.
If I have been taking 200 mg progesterone capsules daily for six months (prescribed by doctor), but I would like to switch to topical because I can no longer afford seeing the doctor, how much of the topical should I start out with?
Hi Leslie, we are unable to advise beyond what Magdalena has covered in the article.
How much progesterone should you use?
It will depend on how low and symptomatic you are, your diet, and stress levels (remember the pregnenolone steal I talked about above?). I recommend to start slow and then dose up.
If you chose to use ProgestPure, start with one full dropper which will give you 20 mg of bioidentical progesterone. You can double that (by doing it twice a day) to 40mg per day if symptoms don’t improve.
If you want to try a higher dosage, I recommend working with a skilled functional practitioner who knows the ins and outs of bioidentical hormones and tests your levels to be sure that you don’t overproduce the “dirty”: progesterone.
I hope this helps!
~ Jeanne HB Team
Each brand is different and may not be as strong as Bioidentical hormones. MACA (cooked/gelatin so it doesn’t block thyroid) is awesome for glands/hormones as it nourishes the glands. NO gluten may help more nutrients absorb as it helps heal the gut lining (stomach/intestines). NO gluten may help glands. Oral maybe destroyed by the liver so topical maybe less needed. A person needs to rotate where they put the cream on the skin. I need all three hormones….estriol/progesterone/testosterone. Herbs may raise hormones also. See herb formulas on Amazon/health food store etc.
So as I was reading the information and really felt like yes I have all the symptoms of low progesterone I need to get some cream! Then as I continued to read it says not to use if you’ve had er, or positive breast cancer; which I did have in 2011 at 46 years old. What can I use then to alleviate the hot flashes, waking at night exhaustion, low sex drive, weight gain, etc…?
Hey Donna,
You may be interested in looking into our Cooking for Balance program, which helps you to restore the health of the gut, liver and sugar level which is the foundation of hormonal balance. https://hormonesbalance.com/cfb/
Healthy regards, HB Team
A lot of good information here, but as a cautionary note, I wouldn’t recommend adding topical progesterone based on symptoms alone.
I took the hormonal quiz offered on this website, which stated that low progesterone was very likely. However, after completing the DUTCH test, it showed my progesterone levels were normal. I do have excess estrogen, which I’m now working to reduce with DIM. When dealing with your hormones, symptoms can certainly guide you, but you need the full picture with proper hormone testing or you can end up doing more harm than good.
Meat/dairy/soy/BPA/chemicals/own fat/The Pill/flax/baby formula etc may cause estrogen dominance. I can’t use DIM…would block my thyroid. At menopause progesterone stops.
I thought saliva testing for hormones was considered best. Why do you recommend urine instead?
Absolutely, salvia testing is best. I am in Integrative Physician who completed a fellowship! 🙂
I don’t have much saliva…dry mouth. The Genova urine test was awesome. Women can figure out their hormone doses by symptoms.
Hi Florie, we prefer the Dutch test (urine) because it gives a complete assessment of the sex hormones and also a comprehensive assessment of what the cortisol or adrenal hormone is doing throughout the day along with some of the metabolites from the adrenal gland. So basically, it’s the most comprehensive test and a great snapshot of where your hormones are at. Saliva is better than blood, it’s just not as complete.
~ Jeanne HB Team
I did a Genova test for hormones…is a urine test. I had to find the right dose of Bioidentical hormones by symptoms..too two years to find the right ratios of estriol/progesterone/testosterone that I need. I needed more than just progesterone.
Hi, I had a partial hysterectomy so I kept my ovaries but don’t know when ,my cycle starts and ends now. I was on progesterone cream before to help with night sweats and such. What do you recommend for determining when to use and when to take the days off since I don’t know when my cycle starts and I don’t fall into the menopausal category yet? Thanks!
HI Lori, Generally speaking for those not cycling, we recommend 3 weeks on, and then 5 days off. You of course would want to talk this through with your health care provider and make sure to talk through how this supplement would work with your current daily protocol. HB Support
I take progesterone nonstop..don’t do a break, but do rotate where I put the cream. I can’t stop it. It is helping my immune system from Lyme/coinfections and makes cortisol which helps my adrenals.
[…] – it is, however, a totally different animal from bioidentical progesterone. Please read Part 1 of the Progesterone Series article that cites all the studies that prove this point. What fuels the cells is either synthetic […]
Ive been taking chaste tree suppliment from standard process for several months now after working with an acupuncturist. I’m wondering if Magdalena will address herbs & their benefit. I’m 46 & still have a regular cycle each month but my luteal phase has definitely shortened each month.
I am 61 years old and had many of the symptoms described during my pre-menopausal years. I still have the symptoms not related to menstrual cycle such as: fatigue, low libido, inflammation, high blood sugar, acne. I have NAFLD and a degree of cirrhosis. Am I a suitable candidate for the progesterone? The best Ive ever felt was during the middle of my pregnancies and the worst was while breastfeeding. Advice please? TIA!
Hey Pam,
While you may want to consider including progesterone in your supplement routine, first and foremost I recommend to take a look at nutrition. You may be interested in checking out Magdalena’s Cooking for Balance program. Restoring the health of the gut, liver and sugar level are the foundation of hormonal balance, which are all addressed in this program. Please feel free to reach out to [email protected] for further support.
Healthy regards, HB Team
Chaste tree is an excellent herb! Magdalena actually offers an entire program called Herbs for Balance that I welcome you to check out. https://hormonesbalance.com/hfb/
Healthy regards,
HB Team
Can Progesterone use increase heartburn/GERD? What are other side effects?
Heart burn can be due to gluten which can hurt the stomach/intestines. Heart burn can be due to low HCl (stomach acid) since gluten hurts the cells of the stomach lining that make stomach acid. Taking HCl and enzymes with meals may prevent heart burn and eating gluten free so the gut lining heals. Progesterone helps the adrenals/thyroid/lowers swelling and inflammation/lowers blood sugar and much more. It is awesome help.
Hi…. Due to prescription of oestrogel(menopause symptoms) I’ve also been told to take one utrogestan orally per night. I’ve started using progesterone cream and find it a lot better for anxiety. Can I discontinue the utrogestan and just use the cream?
Hi Sally,
Thank you for your question but when it comes to prescriptions, it’s better to consult your doctor or a medical professional. Thank you.
Healthy Regards,
HB Team
A strong probiotic before one meal may help the use of food and multiply B vitamins etc. Orthobiotic probiotic helps me.
Yes. When I took the oral progesterone it caused heartburn but the topical spray did not.
The part 2 of this article discusses potential side effects. Please feel free to reach out to [email protected] if you have any further questions after reading the second portion of this article.
https://hormonesbalance.com/articles/topical-progesterone-when-why-and-how-part-2/
Healthy regards- HB Team
Can I used Progesterone cream if I’ve had PR & ER + breast cancer in the past? I’m almost 2 years cancer free.
Hi Alison – please read the article, get educated and decide from there.
How can we find a practitioner where we live. When I ask my primary care dr she looks at me like I am crazy n my gynecologist says they don’t do that n doesn’t know of anyone to refer me to??? I live in New Jersey…when I Google it nothing valet comes up in the search. Please help with how to fund a reference. Tx u.
Hi Cindy, here is a great resource you can use to find an functional medicine practitioner in your area.
https://www.ifm.org/find-a-practitioner/
Hi Thank you for Wonderful Informative articles, Can you please share Natural Herbal ways of Boosting Progesterone or Preglenone ?Foods n Herbs etc?🙏
Hi Manisha!
You may be interested in checking out seed rotation. https://hormonesbalance.com/articles/how-to-use-seed-rotation-to-rebalance-your-menstrual-cycle/
Healthy regards,
HB Team
My daughter who is 20 has adrenal fatigue and, surprisingly, low progestrone. We see a functional medicine chiropractor. He was really surprised to see someone her age with low progesterone. she is getting married and recently began taking birth control. She stopped taking her topical progesterone at that point because of the level in the birth control. She started having anxiety. Should she start with a low dose and see if it helps with the anxiety? Why would someone her age have low progesterone?
Hi-I was hypothyroid and had signs of low progesterone from my low 20s, when I began tracking my cycles-I’m sure there were multiple contributors, but I believe that a major contributor was significant weight loss/near anorexia my senior year of high school-I then began to have signs of low progesterone (acne) poor thyroid function-problems with weight gain. She might consider fertility awareness for family planning-hormonal birth control negatively impacts thyroid function and hormonal health.
Hey Batrice,
Thank you for your input! To add it it, you may be interested in checking out this article on birth control. https://hormonesbalance.com/articles/pill-can-seriously-affect-womans-health/
Wendy, your daughter may be interested in looking into our Cooking for Balance program. Restoring the health of the gut, liver and sugar level are the foundation of hormonal balance. If she focuses on these first, she very likely will experience higher progesterone production as well. https://hormonesbalance.com/cfb/
Healthy Regards, HB Team
Hi! I have taken the DUTCH test and results have shown low progesterone at age 30. I also have symptoms (acne, anxiety), but I’ve never taken birth control and I am not underweight. Does anyone know any other causes of low progesterone in my age group or what foods/herbs/supplements support it before trying a topical?
Hi Kalli,
I definitely recommend checking out our article “10 Natural Ways to Boost Progesterone’. If you have any further questions, please feel free to reach out to [email protected] and we would be happy to assist you.
https://hormonesbalance.com/articles/10-natural-ways-to-boost-progesterone-balance-hormones/
Healthy Regards,
HB Team
Hi Wendy,
What testing method did your daughter’s functional chiropractor use? Magdalena recommends the DUTCH urine test. There could be many things at play here, including birth control and stress, which is a huge progesterone robber. Your daughter’s functional doctor will likely have a plan to address the root cause. Once that is addressed the other issues usually fall into place. That being said, she may want to look at some of Dr Jolene Brighten’s (friend of Magdalena’s) work on post birth control syndrome.
Please reach out to us by email if you want to discuss further.
I just started taking this last week and have had extreme bloating and gas. Do you think this is a coincidence or from the progestpure? i do not eat wheat or dairy. I could have had some exposure a few days ago but it’s really intense. I am 50 and post menopause and have not registered in blood work really any hormones for at least 5 years. Never took bio identical hormones.
Hi Charlee,
Bloating and gas is not a side effect that we hear about from Progestpure, but everyone is different so we cannot say for sure that it is not related. It could be a coincidence, but to be sure you might want to taper off your progesterone and see if your condition improves.. After taking some time off, you might want to try it again to see if the gas comes back. And it is always best to check with your naturopath or functional doc first.
HI I was told to take up a troche of progesterone of 75mg. But instead I want to go down the cream path. However they can’t tell me what that translates too in a cream. How can I find out?
[…] progesterone may also lead to hot flashes. Progesterone is a hormone that helps balance the effects of estrogen […]
[…] possibly potassium. No matter what, make sure you’re eating plenty of potassium-rich vegetables. Progesterone cream is also highly recommended to address estrogen […]
If the metabolites from the pill form cause anti-anxiety benefits, why would you not want those? I just learned about this. I currently take the cream at night which knocks me out but then I wake up a few hours later and can’t go back to sleep. I learned that Some women take the pill as well as the cream form so they can then sleep through the night. Why would this be a bad thing? I’ve also learned that it’s usually recommended to take the pill form if you’re also taking estrogen because the pro cream doesn’t quite balance out the negative effects of estro, but the pill form does.
Anyway, I’d like to learn more about the positive effects of the pro pill!
I have just gone through 2 miscarriages in a row (both at 6 weeks) due to low progesterone. When’s the best time to use progesterone in my cycle? And also during the pregnancy so I can hold the pregnancy next time?
Also, when and how do I taper if off progesterone during pregnancy so I don’t induce a miscarriage?
Hi Jules, we’re sorry to hear that you have going through fertility challenges. If you could please send us an email at [email protected] it will be easiest for us to provide some insights for you. Thank you! ~HB Support
I take Estrogel daily and was prescribed Prometrium caps every night 100mg. I have tried to take the prometrium caps for almost 2 months now but every night, one hour after taking them, I start to feel totally drugged, extremely dizzy, fatigued and almost nauseous. I cannot even walk to the bathroom because I feel so bad. I also get horrible nightmares after taking the oral prometrium.
I cannot continue like that. I live in Canada so cannot really get your product, but I have still 2 months worth of oral prometrium pills and read somewhere that I could pierce the capsule and squeeze out the milky contents and apply on the skin.
Do you think this could work? otherwise I will have to stop the oral pills because I do not want to continue living like a Zombie.
I do not have the option of seeing an MD that knows about bio identical hormones.
I am post menopausal
My second question is: Do topically applied progesterone creams still protect the uterine lining and prevent uterine C?.
Hi Sonia, we cannot speak to your medication and if it can be topically applied. If there was a way for you to see a naturopathic doctor or other functional medicine doctor in Canada who could guide you, this would be a perfect question for them.
As for topical progesterone, since it is supporting healthy progesterone levels in the body, it has the same benefits as other natural progesterones so the uterine lining would also see potential benefits as well. ~HB Team
I’m really worried about progesterone working on gaba receptors. Been on for a year and also been on benzos for 4 years daily use. They both work on gaba. I know the benzos have some damage but I think they are cross tolerant to eachother or having some kind of reaction. I tried coming off oral progesterone so many times and was unsuccessful each time. Got severe withdrawals similar to benzo withdrawals. Severe depression, akathisia, panic attacks, severe weakness, migraines, motility issues. What do I do? Is there a way to taper oral progesterone? I’m gonna stay on for a bit until I’m off the benzo but really worried my gaba receptors are damaged bc I have akathisia. Also does topical progesterone hit gaba? Thank you
Hi Lauren, since we are not medical professionals, we aren’t able to make inferences on what to do in your individual case. We would recommend consulting with a functional or integrative practitioner to support you with these questions and the best route moving forward. We understand how difficult and complex these experiences can be and hope you’re able to consult with someone to support you needs. ~HB Support.
Can you lighten painful period cramps and other symptoms by taking it? Would you take it the same way; day 14-27 of your cycle?
Hi Michaela, yes, this can help with uncomfortable periods. The best way is to use in the last half of your period until day 1 of your menses. ~HB Support
Hello, I placed an order on line, do you ship to Canada? The order won’t process and I want to purchase the cream.
Thanks
Hi Elyse, unfortunately, we do not ship to Canada. You can check into the third part shipper myus.com but should also check customs as some countries do not allow for progesterone cream to be shipped in. If this is the case, then you can look into compounding pharmacies or for a brand that excludes the above ingredients from the section “How to Choose Your Topical Progesterone”. ~HB Support
I am a bit confused. Black Cohosh is supposed to help with hot flashes yet that increases estrogen. This article talks about progesterone as being the key to stop all those symptoms. Is there an article that explains the difference?
Hi Sally, black cohosh helps increase estrogen as an adaptogenic herb which means in cases where there is low estrogen it can help boost those levels, and in women who have hot flashes due to drops in estrogen, this herb can help keep levels from dropping. If your hot flashes are coming from an imbalance of estrogen and progesterone, than using topical progesterone could be more beneficial. Check out our hot flashes article for more explanation. https://hormonesbalance.com/articles/hot-flashes-symptoms-causes-solutions/ ~HB Support
Is the Wellena cream USP progesterone? The ingredients say Micronized Progesterone (from Wild Yam).
Great article
thank you
My question is: I am 49 yrs old and have no health issues described above, however i am having a lot of symptoms in my hormones and my cycle . So last year once in july , my menstruation was late 38 days. And then it arrived after 38 days
This month it’s late again, 10 days now. Not Pregnant
However my Periods have been regular 25-31 days up until this month, i don’t know what’s happening
I have been taking oral progesterone before, and progesterone cream. At this time i don’t take oral, just the cream. I don’t know how do i use the cream since my cycle is irregular
Doctors are impossible to deal with, hence i don’t go to them
they don’t know anything .
I take Maca peruvian for perimenopause and other supplements to support my condition
please help me to figure out my situation
at least any suggestions would be appreciated
thank you
HI Elka, irregular cycles can be signs of Peri-menopause. The average woman goes through menopause (the cessation of cycles for one year) at age 51. That said, it is not uncommon to see variations in cycle length and frequency in our late forties and early fifties. You might look into supporting both estrogen and progesterone to see if that is right for you. Take care! HB Support
What is the recommendation for progesterone application for those struggling with edema from Hypothyroidism? I had a test years ago for my hormones and [ZRT Labs] said I wasn’t absorbing my topical progesterone, likely due to edema fluid blocking it. Thanks so much!
Hi Megan, Thank you for reaching out. We don’t have guidelines for those dealing with edema, so would recommend you reach out to your practitioner. Thank you! HB Support
I’ve looked everywhere but can’t find the reasoning why menopausal women need to use natural progesterone cream for 25 days out of the month. I’ve read Dr. Lee’s books and can’t find an answer anywhere! Thank you!
Hi Amanda, the reasoning is to mimic a traditional cycle giving the receptors a break, so that their absorption stays optimal. Without the break, over time, the receptors may not absorb as well, and the bioidenticals may not work as well, or could stop working. I hope that helps. Jen @HB Support
I’m 65, post menopausal and a 15 yr. BC survivor that was ER/PR+..
I’m also hypothyroid, no meds. I need help balancing my hormones. Is there anything I can do?
I’ve learned applying bioidentical cream is more beneficial applying it to our vaginal lips per Dr. Jonathan V. Wright, a well-known pioneer in natural medicine, researcher, author and speaker who runs the Tahoma Clinic and has provided evidence-based natural treatments to thousands of patients. “If you apply the cream to your mucous epithelial membranes that line your uterus and vagina you obtain a virtually ideal administration system. Not only is absorption through these membranes more complete than through your skin, but hormones absorbed through your vaginal membranes enter the very same pelvic plexus of veins that your ovaries normally empty into. From here the hormones are carried to your heart and lungs and distributed to your tissues just as if your ovary had actually produced them.”
Hi I had a blood clot in my lung and now I have to take Eliquis a blood. Can I take this or is there a rest for me to take? I have everything hot flashes, gaining weight mood swings sadness no sex drive at all. I do need some help, but I am not sure if I can take it.
Hi Kerstin, we are not medical professionals, so can’t give specific advice on that. That is a great question for your practitioner to discuss further. Take care – Jennifer @HB Support
This product sounds great and is something I would like to offer to my patients. Do you offer professional discounts or whole sale pricing or an affiliate program so that I can sell this in my center?
Hello Dr. Petrucci, yes, we have wholesale opportunities. You were welcome to reach us at [email protected] and we can get you in touch. Thank you! Jennifer @HB