What You Will Learn in This Article
- Symptoms of hot flashes
- Triggers of hot flashes
- Potential mechanisms/causes
- Why some women suffer more
- Solutions for hot flashes
Hot flashes are the bane of many a peri- or post-menopausal woman’s existence – especially since they are linked to insomnia and depression. Because they have such a negative impact on quality of life, they are one of the most common reasons women make doctor appointments while in their forties and fifties. The typical age range for developing moderate-to-severe hot flashes is between the ages of 45 and 49. They tend to last for an average of ten years.
While the mechanisms behind this irritating symptom aren’t fully understood, diet and lifestyle changes may help. There’s also a promising supplement based on researched botanical extracts that may help. This article will give you some things to consider and some tips for lessening both the frequency and severity of hot flashes.
What do Hot Flashes Feel Like?
Hot flashes tend to come on suddenly (hence, “flash”) and involve a number of distressing and uncomfortable symptoms:
- Sudden warmth of face, neck, and chest
- Sweating
- Increased pulse rate
- Chest tightness
- Anxiety
- Flushed skin, sometimes blotchy
- Sometimes followed by a chill
If it’s not enough to have these unpleasant mini sauna sessions during the day, they are often accompanied by night sweats that wake you from a pleasant slumber. This can lead to insomnia, sleep deprivation, and feelings of hopelessness and depression.
Hot Flash Triggers
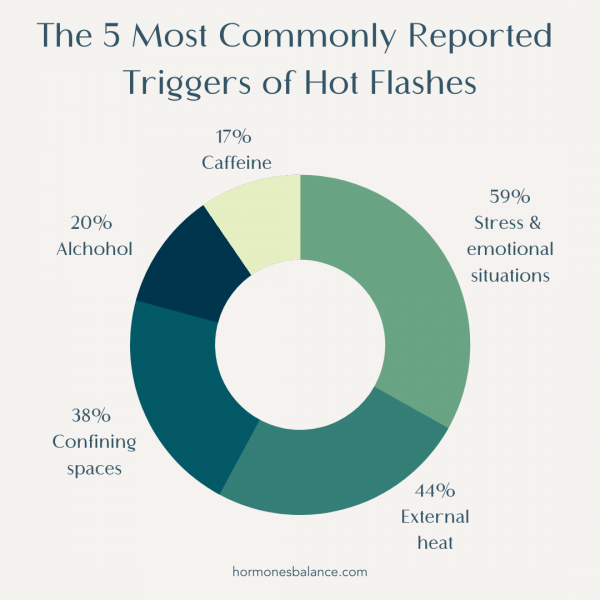
If you’re not sure what triggers you, consider keeping a small notebook in your purse. Then make note of when hot flashes come on and what happened right before. The 5 most commonly reported triggers of hot flashes are the following:
- Stress/Emotional situations (59%)
- External heat (44%)
- Confining space (38%)
- Alcohol (20%)
- Caffeine (17%)
Note that these triggers simply bring on a hot flash. They aren’t actual causes of the imbalance. I, therefore, looked deeper into what the underlying causes of hot flashes were. It turns out, there are at least seven, most of which you can control.
7 Causes of Hot Flashes
The mechanism isn’t completely understood, but medical experts believe hot flashes originate in the brain and are caused by the dysregulation of the temperature control mechanism in the hypothalamus. Certain hormones/catecholamines, adrenaline (epinephrine), noradrenaline (norepinephrine), as well as thyroid hormones are likely involved.
While there is a genetic component, the actual causes behind dysregulation in the hypothalamus are related to some type of imbalance or deficiency:
1. Blood Sugar Imbalance
Essentially, what this means is that anything that puts stress on the brain and body can be a contributor to hot flashes. That includes blood sugar issues and hypoglycemia. Studies have found that a drop in blood sugar can trigger hot flashes. Women were more likely to have hot flashes if they went a longer time between meals.
When I was in private practice, I worked with Dr. Francis, an emergency room physician. She used to experience debilitating hot flashes at exactly 11:00 a.m. each morning. The problem was that they would strike in the middle of her shift when she often was saving lives. Something had to change. After initial reluctance, she sent me her food journal, which said that her 8:00 a.m. breakfast consisted of cereal, topped with fruit and yogurt. She had also noted that if she had a handful of walnuts (full of protein, fat, and fiber!) around 10:45 a.m., she wouldn’t get a hot flash. That was a great observation; one that proved her dropping blood sugar around 11:00 a.m. was the cause of her hot flashes.
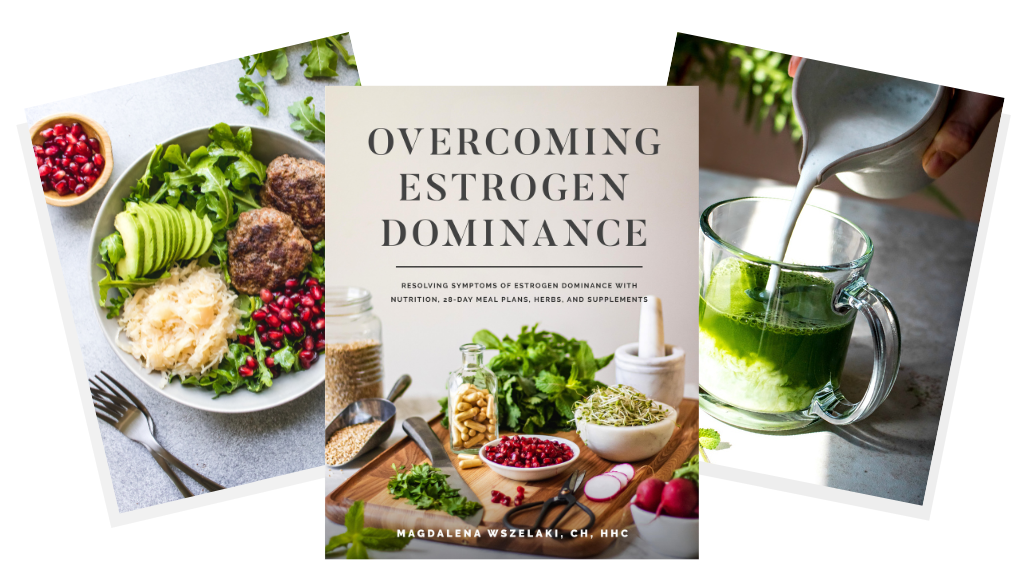
Because of her work, she wasn’t always able to snack to prevent a hot flash. I wanted to focus on the bigger picture, anyway, preventing her blood sugar levels from dropping in the first place. We changed her breakfast to a PFF (Protein, Fat, Fiber) kind of breakfast, and her hot flashes immediately stopped. This is why most of the breakfast recipes in my books (including Overcoming Estrogen Dominance) are based on the PFF principle.
2. Low or Dropping Estrogen Levels
It is no surprise that hot flashes are most common in women entering peri- or menopause because that’s when estrogen production starts dropping. However, it can occur earlier, before age 40, in those who are dealing with primary ovarian insufficiency. In this case, the ovaries aren’t working properly and can’t release adequate estrogens and other hormones. This is another potential cause of low estrogen levels.
How do you know if you have low estrogen? You’ll want to do a DUTCH hormone test to know for sure, but symptoms of low estrogen include:
- Hot flashes
- Weak bones
- Osteopenia and osteoporosis
- Poor sleep
- Sagging and/or dry skin
- Hair thinning or loss
- Weaker cognitive functions, such as forgetfulness
- Vaginal thinning and dryness
- Incontinence
- Loss of sex drive
- Irregular periods or no periods
What researchers are learning about estrogen is that it’s important to have a balance of estrogen-promoting and estrogen-limiting activities for us to have healthy hormone levels. Both estrogen dominance and low estrogen can be a problem, and that’s where taking phytoestrogens from plants like flax and hops can help. Phytoestrogens can serve as weak estrogens that can help support low estrogen levels, yet replace more potent estrogens so that we don’t become estrogen dominant.
While scientists don’t know exactly why low estrogen levels can cause hot flashes, I believe that blood sugar imbalance and inflammation, when combined with dropping estrogen levels, is the perfect storm.
The good news is that there are food and supplements that can raise estrogen levels – we’ve written a whole article about it.
3. Low Progesterone
Progesterone is also likely involved in hot flashes. Estrogen can cause anxiety when out of balance with progesterone, as progesterone has an anti-anxiety effect on the body. As progesterone levels decline and fail to balance estrogen, the body is also put in more of a stressed, high adrenaline state. Again, stress is the top trigger associated with hot flashes.
4. Inflammation
Additionally, low-grade systemic inflammation has been tied to hot flashes. What can cause chronic systemic inflammation? Certainly, dietary choices – an inflammatory diet or eating foods that cause inflammation in an individual (like food allergies or intolerances) can lead to chronic inflammation.
A study of postmenopausal women and diet found that those who consumed a higher antioxidant diet had fewer hot flashes. Read more about inflammation and how to reduce it in this article.
Many women in our Hormones Balance community have reported a reduction of hot flashes with a change of diet – especially after removing inflammatory foods, such as gluten and dairy, and reducing their intake of sugar and coffee (or completely cutting out all caffeine).
5. Mineral Deficiencies
Mineral deficiencies, such as magnesium, and possibly zinc and selenium may also contribute to hot flashes.
6. Ethnicity
A study of over 16,000 American women found that African Americans and Hispanics were more likely to experience hot flashes than other ethnic groups, including Caucasians. The distribution of women likely to have hot flashes was as follows:
- African American (46%)
- Hispanic (36%)
- Caucasians/Whites (31%)
- Chinese (21%)
- Japanese (18%)
7. Lifestyle factors: Smoking
Smoking is one of the few lifestyle factors that is consistently associated with hot flashes. Women who smoke are more likely to experience hot flashes than nonsmokers. In fact, over the course of 6 years, smokers had a 60% increased risk of vasomotor symptoms like hot flashes as compared to nonsmokers.
Even though hot flashes aren’t fully understood, there are still a number of things you can do to lessen the frequency or severity of hot flashes… or to eliminate them altogether.
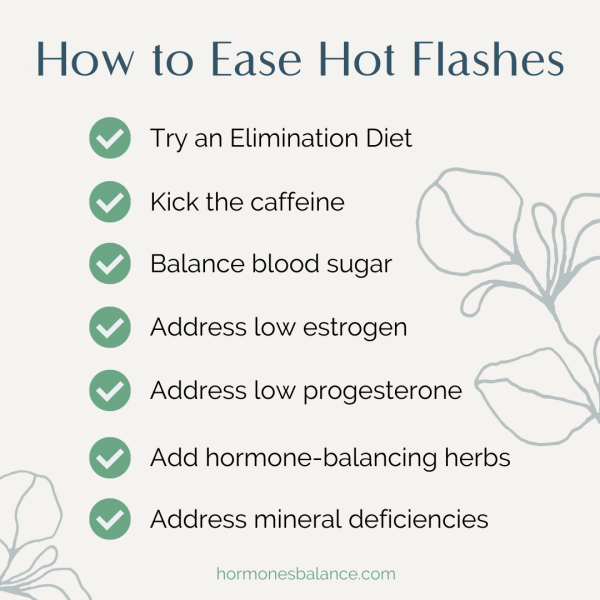
Solutions for Hot Flashes
Diet (Elimination Diet)
Diet is really important here. Hot flashes are yet another sign of hormone imbalance, and my first line therapy for balancing hormones has always been food. (Hence, the creation of my book, Overcoming Estrogen Dominance).
Here are some things to consider:
- Is your diet generally inflammatory or anti-inflammatory?
- Are you intolerant to some of the otherwise healthy foods you’re eating? Gluten and dairy are common culprits.
- Is your diet causing blood sugar dysregulation?
- If you answered “yes” to any of the above, you may want to consider trying an Elimination Diet.
Elimination Diet
An Elimination Diet, which removes potentially inflammatory or allergenic foods, may be the best way to start. There are many versions of this, such as Whole 30, the Paleo Diet, the Autoimmune Paleo Dietl, the Wahls Protocol, the Virgin Diet, etc. Generally, the idea is to remove dairy, soy, gluten, corn, sugar, alcohol, and processed foods. Some versions may also remove eggs, nuts, nightshades, grains in general, legumes, and more.
An elimination diet at its most restrictive lasts only 4 to 6 weeks, and then the diet is expanded. If reactions occur after re-introducing a food, the person is most likely intolerant to that food. Healthy foods causing reactions are removed from the diet until health is improved and the immune system is more in balance.
Many of our program participants have said that after starting the Elimination Diet, their hot flashes disappeared.
Kick the Caffeine
When addressing hot flashes through diet, I hate to break it to you, but it’s really best to also remove coffee. Unfortunately, coffee contributes to Estrogen Dominance, and, according to this study, caffeine may increase blood sugar levels.
In my experience, many women who have given up coffee and caffeine report better sleep within days, fewer hot flashes, and other benefits over time.
Here’s an article I wrote with tricks I used to give up coffee while reducing the side effects. It will help guide you through the process of weaning yourself off caffeine.
If you need a great coffee substitute, try my (Better Than Coffee) Chicory Latte recipe or Rasa from our partner which is an adaptogenic “coffee” that energizes without the caffeine.
Balance Blood Sugar
Unbalanced blood sugar levels can cause the body to stay stuck in an inflammatory state, leading to the overproduction of stress hormones and then a general state of hormone imbalance, including estrogen dominance. We know from studies that blood sugar problems and inflammation can contribute to hot flashes.
To balance your blood sugar, I recommend starting your day with a PFF breakfast. PFF stands for Protein, Fat, and Fiber and is the first step in eating to promote balanced blood sugar levels. Learn more about balancing blood sugar to balance hormones (and grab some great recipes) here.
American Ginseng, cinnamon, and green tea extract are some of the plants and herbs renowned for up-regulating insulin receptors, which then help to balance blood sugar levels. When you combine it with a low-sugar diet, your blood sugar levels are bound to stabilize quickly and you may kiss hot flashes goodbye. Our Wellena Gluco Maximus contains these herbs (and more) and has been a very popular product with our community.
Tip: If you’re experiencing symptoms of estrogen dominance, you can find out more by taking my Free Estrogen Quiz here.
Reduce Inflammation
When you implement all of the above suggestions, your inflammation levels are bound to come down. If you feel like you need additional help in lowering inflammation, try adding GLA Maximus which contains GLA, or gamma linolenic acid (the very substance that’s made Evening Primrose oil so famous – except we use Borage Oil because it contains higher GLA levels); it’s designed to help balance the body’s inflammatory response by increasing the activity of the anti-inflammatory prostaglandins.
Address Low Progesterone
Low progesterone may also lead to hot flashes. Progesterone is a hormone that helps balance the effects of estrogen in the body. It’s very sensitive to stress in our lives. There are a few nutrients that can help boost your progesterone naturally; however, for many women, topical progesterone is a more efficient way to raise your progesterone to healthy levels. This study found that a form of progesterone reduced hot flashes by up to 80%.
ProgestPure, by Wellena, is a natural and clean topical progesterone serum providing 20 mg of bioidentical progesterone in each 1 ml dose. This highly bioavailable form of progesterone contains four ingredients: micronized USP progesterone, dimethyl isosorbide, Caprylic/capric triglyceride (from coconut), and vitamin E. It’s free of parabens, mineral oil, and petroleum. We also now carry a cream-based ProgestPure, which provides 25 mg of bioidentical progesterone per serving and is quickly becoming a customer favorite.
The progesterone used in ProgestPure is super-micronized and is delivered in a proprietary triglyceride carrier which helps the progesterone absorb more efficiently as compared to conventional creams. This serum also contains a natural sugar-based complex, dimethyl isosorbide, which increases progesterone solubility and helps the progesterone penetrate more deeply through the skin and at a faster rate.
Additionally, the dimethyl isosorbide helps preserve the potency of the progesterone after manufacturing. This is in contrast to water-based products, which can lose as much as 30% or more of their potency within the first 60-90 days after manufacturing.
Women going through perimenopause, menopause, and post-menopause and who suffer from hot flashes can use topical progesterone for 25 days out of a 30-day calendar, with 5 days off. If you are in peri-menopause and still menstruating, start progesterone 5 to 7 days after the first day of your period and continue until the next period.
You can find our ProgestPure Oil and try it for yourself here. If you prefer a lotion base instead of oil, shop ProgestPure Cream here.
Increase Low Estrogen
Low estrogen is another hormonal contributor to hot flashes. Phytoestrogens, estrogens naturally occurring in plants, may be the best natural solution. A review of 62 studies using plant-based therapies for menopause symptoms in 6653 women found that phytoestrogens, such as lignans found in flax, helped reduce hot flashes.
There are three types of phytoestrogens:
- Lignans (including enterolactone and enterodiol)
- Isoflavones (genistein, daidzein, and biochanin A)
- Coumestans
The highest concentration of phytoestrogens is found in lignans. In humans, 7-HMR is a precursor to the lignan, enterolactone. Enterolactones are associated with a healthy immune system, cardiovascular fitness, balanced blood pressure, healthy prostate and breast health, strong bones, and balanced hormones.
In an eight-week study of 22 menopausal women, HMRlignan was given at either 36 mg per day (low dose) or 72 mg per day (high dose). The high dose group went from an average of 28 hot flashes a week at the beginning of the study to 14.3 per week by the end of the study. The 7-HMR supplement had reduced them by half.
A phytoestrogen called 8-prenylnaringenin (8-PN) is the most potent scientists have found yet. Researchers have found 8-PN to support a healthy transition to menopause, plus, cardiovascular fitness, healthy breasts, strong bones, and healthy tissue in general. In a study of 8-PN from standardized hop extract (100 mcg per day) menopausal women were given either the hop extract or a placebo for 16 weeks. The hop extract helped lower symptoms, including hot flashes.
Several other studies confirm how well these particular hops extract works in reducing menopausal symptoms like hot flashes. And it goes beyond alleviating uncomfortable symptoms.
According to a study on hot flashes and associated risk factors,
“Hot flushes may possibly mark underlying vascular changes that are associated with subclinical cardiovascular disease, increased aortic calcification among users of hormone therapy, greater incident coronary heart disease, and may be a risk factor for poor bone health.”
8-PN may help women maintain a healthy cardiovascular system with normal blood flow.
Researchers also looked at 8-PN’s potential for protecting women’s bones. They found that 8-PN supplementation had results that were similar to hormone replacement. It improved movement and increased Bone Mineral Density. (BMD).
This extract is a great all-around supplement for women’s health as we age.
Wellena’s supplement, Estrogen Boost, contains both 8-PN and HMRlignan, delivering a powerful clinical blend of phytoestrogens to support healthy natural estrogen levels. This blend supports natural aromatase activity, which helps convert androgens to estrogen. It may also raise “good” estrogens while blocking “dirty” estrogens, relieving hot flashes and other symptoms of low estrogen. It may also support natural breast tissue health.
As a side benefit, this supplement also supports a healthy cardiovascular system, healthy blood sugar levels (alongside a healthy diet), a balanced immune system, strong bones and skin, and even aid in attaining restful sleep. While supplements can’t mitigate disease, they can certainly support optimal health in all the systems of the body.
Ingredients include:
- Hops flower (Humulus lupulus) – Contains potent phytoestrogens and healthy aromatase properties
- Norway Spruce (Picea abies) – Contains “good” estrogens while blocking “dirty” estrogens

FAQs
Q: Can I take this product if I have Estrogen Dominance?
A: Yes. This product raises “good” protective and gentle estrogens. Estrogen Dominance occurs when the body produces too many “dirty” estrogens or when there is a deficiency in the estrogen-to-progesterone ratio.
Q: What’s the difference between flaxseed and Estrogen Boost?
A: Flaxseed also contains phytoestrogens; however some women develop digestive troubles from consuming it – in which case Estro Boost might be a better option.
You may also want to experiment with Reishi mushrooms, which were shown in a study to naturally regulate low estrogen levels associated with menopause. Other herbs also support a healthy estrogen balance. You can enjoy them as herbal teas or as ingredients in healthy recipes:
Herbal Recipes for Hot Flashes
Certain herbs have been shown to be helpful for cooling those hot flashes:
- Dong Quai – available as a supplement, but you can also incorporate them into your food like with these Dong Quai Almond Butter Cups.
- Chaste berry (otherwise known as Vitex) – Found in Wise Women’s Balance. You could also try our Chasteberry and Rose Tea recipe.
- Black cohosh – This is also found in Wise Women’s Balance.
- Red clover – Try our Calming Hot Flash Latte with Red Clover.
- Maca – Learn if maca is right for you by reading this article.
Address Mineral Deficiencies
Mineral deficiencies may also contribute to hot flashes. Try adding magnesium in the form of magnesium glycinate. A small 2011 study of 29 women published in the journal, Supportive Care in Cancer, found that supplementing with 400 to 800 mg of magnesium per day helped reduce the frequency and intensity of their hot flashes over a 4-week period.
The study used Magnesium oxide, which I don’t recommend, due to its low bioavailability (only 4%). The highly bioavailable Magnesium glycinate is a much better bet. Read up on how magnesium impacts your hormones and why I don’t recommend magnesium oxide by reading Which Form of Magnesium is Right for You?
In Summary
Remember: Take away before you add. Remove the high carb, inflammatory, glucose-spiking foods. Remove foods you are sensitive to. Lower your stress and inflammation. Add in colorful whole foods, and, as you start Overcoming Estrogen Dominance, include some of the recipes listed above.
Try balancing your hormones with quality supplements. We hold all of our Wellena supplements to the highest standards, but if you’re looking for one to start with, I’d highly recommend the Estrogen Boost, due to its all-around balancing and rejuvenating effects.
The body has an amazing ability to heal. We just need to give it the right resources. As you become more balanced, your hypothalamus and thermostat will balance, too.
Learn more with Overcoming Estrogen Dominance
“The body has an amazing ability to heal. We just need to give it the right resources.”
In Overcoming Estrogen Dominance, my goal is to empower and give you the tools to take control of your hormones and health.
More than 70% of women experience estrogen dominance. The symptoms range from lumpy and fibrocystic breasts to thyroid nodules, hot flashes, fibroids, uterine polyps, painful, heavy or irregular periods to infertility and miscarriages, from mood swings to insomnia, weight gain to fatigue.
So many women have experienced the pain and frustration that comes when they feel their symptoms and complaints are dismissed or minimized. This is particularly true for women who are experiencing the symptoms of hormone imbalance. Even when doctors do offer treatment, it’s typically in the form of prescription medication or invasive surgical procedures.
In Overcoming Estrogen Dominance, I hope to show that those extreme interventions are often unnecessary, and to give women a roadmap to reverse estrogen dominance using food, herbs, supplements and natural protocols to rebalance hormones.
To get your copy of Overcoming Estrogen Dominance, go here.
Resources
Hays, Bethany. Female Hormones: The Dance of the Hormones, Part I. The Textbook of Functional Medicine. 2010.
Ziv-Gal, A. et al. Factors that may influence the experience of hot flushes by healthy middle-aged women. Journal of Women’s Health. 2010.
Gold, E.B. et al. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40–55 years of age. American Journal of Epidemiology. 2000.
Thurston, R. C. and Joffe, H. Vasomotor symptoms and menopause: findings from the Study of Women’s Health across the Nation. Obstetrics and Gynecology Clinics of North America. 2011.
Dormire, Sharon and Howharn, Chularat. The effect of dietary intake on hot flashes in menopausal women. Journal of Obstetric, Gynecologic, and Neonatal Nursing. May/June, 2007.
Mayo Clinic Staff. Hot flashes. Mayo Clinic website. 2018.
Smith, Rebecca L. et al. Factors Associated with Poor Sleep During Menopause: Results from the Midlife Women’s Health Study. Sleep Medicine. 2018.
Zeleke, B. M., et al. Vasomotor symptoms are associated with depressive symptoms in community-dwelling older women.
Menopause. June, 2017.
Franco, Oscar H. et al. Use of plant-based therapies and menopausal symptoms: a review and meta-analysis. JAMA. June 2016.
Park, H. et al. A pilot phase II trial of magnesium supplements to reduce menopausal hot flashes in breast cancer patients. Supportive Care in Cancer. 2011.
Huang, Wan-Yu et al. Circulating interleukin-8 and tumor necrosis factor-α are associated with hot flashes in healthy postmenopausal women. PLOS one. August, 2017.
Abshirini, M. et al. Dietary total antioxidant capacity is inversely related to menopausal symptoms: a cross-sectional study among Iranian postmenopausal women. Applied Nutritional Investigation. March, 2018.
Lam, Michael. The Role of Adrenal Fatigue in Estrogen Hormone Dominance. DrLamCoaching.com. Accessed February 24, 2020.
Pizziol, A. et al. Effects of caffeine on glucose tolerance: a placebo-controlled study. European Journal of Clinical Nutrition. November, 1998.
Shanafelt, T. D. et al. Pathophysiology and Treatment of Hot Flashes. Mayo Clinic Proceedings. November, 2002.
Shimizu, K. Estrogen-like activity of ethanol extract of Ganoderma lucidum. Journal of Wood Sciences. 2009.
Feature photo by Trent Szmolnik


Great article, thanks. At present, the onset of menopause often coincides with a woman reaching a certain standard of living – the prevailing family environment, career success, and high self-esteem. And hormonal changes disrupt the usual course of things, affecting well-being and attitude. Before modern medicines appeared on the shelves of pharmacies, many preferred steadfastly to endure all the symptoms of the extinction of reproductive function. Others – resorted to the help of folk remedies, often ineffective and even dangerous. But now there is no need for such extremes because reducing to a minimum of discomfort after menopause is possible with the help of modern medicines. Good luck!
I (72 year-old woman) ave been on biodentical hormones through a “specialist” ; unfortunately, the cost & distance of the provider & a new inexpensive all-in-one pill format called Bijuva, plus some other supplements (I think) got me to have hot flashes when I never had before! Now off them & trying to get straightened out. Problem is a very substantial absence of knowledgeable & affordable people in this field, particularly in rural Minnesota😩
Hey Chally,
Many clients have had success with a functional medicine doctor. If you need help locating one in your area, here is a good tool:
https://www.ifm.org/find-a-practitioner/
Also, please feel free to reach out to us at [email protected].
Healthy Regards,
HB team
i am not sure I trust the quiz. I am very fit, low body fat, have lean solid muscle. I am 49 and blessed to still be taken for someone in her mid-30’s. I do supplement to keep testosterone up to keep muscle. In all my decades i have lost period due to low body fat/lean muscle. I often get night sweats from hot memory foam bed and whenever i’m super fit I sweat more in my sleep. This is the longest at 4 months without. I doubt it is estrogen dominance. it confuses me..does low estrogen or high estrogen cause hot flashes?? Not sure if i should take more estrogen or less…do i try the progesterone cream? all of this is new and confusing. I feel great and only dealing with short occasional hot flashes/night sweats and no period. How do i know for sure?
Hi Jozie, one way would be hormonal testing. Magdalena refers people to https://yourlabwork.com/hormonesbalance/ This is a great resource since can order the tests from that site yourself. For a complete breakdown and exploration into hormonal balance and Estrogen Dominance, I would encourage you look into her Estrogen Reset program. It also provides ways to use foods, herbs and supplements to restore balance, and includes a protocol for absent & irregular periods.Here is the link for you see if this may be a good fit: https://hormonesbalance.com/join/
Such a great article. It very knowlegable and helpful. Thanks for providing this information. Please include https://www.menopauset.com/ in you list I would appreciate it greatly.
Can you take wise woman balance and Estrogen boost together? Or you need to take one or the other? And how would I take them , if both can be used?
I was wondering if you had a recommendation for a hormone panel blood test. I think before adding a bunch of supplements and trying to guess what is wrong. A hormone test would be recommended so you are adding in the correct supplements or real food to balance out everything.
Also with breast cancer I would think it would be different recommendation than someone who is in menopause their are certain medication interactions that could take place and breast cancer patients need to be careful. Tamoxifen and black cohosh has a reduction in the medication-most people are not aware of that.
Hi Pam, for hormone testing Magdalena refers people to https://hormonesbalance.com/articles/what-lab-tests-to-order-to-manage-your-hormones/ You can order the tests from that site yourself. It is important to find a skilled physician to interpret those results. It is especially important to consult with an integrative or functional practitioner with a history of breast cancer prior to making any supplemental changes. ~HB Support
Hi Jocelyn, our supplement specialist informed us that it is ok to take both of these products together. Using them based on their recommended serving size is best unless otherwise directed by your healthcare practitioner.