
What You Will Learn in This Article
- What does it mean to have high blood sugar?
- What are the symptoms of high blood sugar?
- What does it mean to have low blood sugar?
- What are the symptoms of low blood sugar?
- How does imbalanced blood sugar impact hormones?
- What should your diet look like for supporting balanced blood sugar levels?
- Which supplements can best support balanced blood sugar?
Ever feel energized first thing in the morning and then crash around 10 or 11am? How about in the afternoon? Do you find that you feel great at lunchtime or immediately after, but then start to glaze over within the next few hours? This isn’t uncommon, but it isn’t normal, either.
High blood sugar levels, followed by low blood sugar has become all too common today. The highs and lows of a diet high in simple sugars has set us up for episodes of hypoglycemia, weight gain, and hormone imbalance.
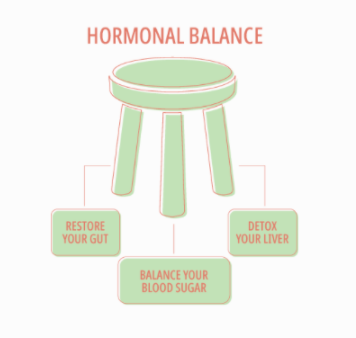
In my books, Overcoming Estrogen Dominance and Cooking for Hormone Balance, I talk about hormonal balance relying on three legs of a three-legged stool. These legs are Digestive Health, Liver Detoxification, and Blood Sugar Balance.
In this article, we’ll cover how to know whether you’re suffering from unbalanced blood sugar levels, how that can impact your hormones, and what you can do about it. So, let’s get started.
What Does it Mean to Have High Blood Sugar?
The official textbook definition of high blood sugar (hyperglycemia), according to the National Institutes of Health (updated 2021) is:
“blood glucose greater than 125 mg/dL while fasting and greater than 180 mg/dL 2 hours postprandial. A patient has impaired glucose tolerance, or pre-diabetes, with a fasting plasma glucose of 100 mg/dL to 125 mg/dL. A patient is termed diabetic with a fasting blood glucose of greater than 125 mg/dL.” (1)
However, if your blood glucose test results show levels greater than 90 mg/dL (even though labs/doctors will say 99 mg/DL is acceptable), you’re already too high.
Testing results that indicate high blood sugar levels include the following:
- Blood glucose over 90 mg/dL
- HA1c over 5.4 (even though labs/doctors will say 5.6 is okay)
- Insulin over 15 IU/mL (even though labs/doctors will say 24.9 IU/mL is okay)
If test results show numbers over the ones mentioned above, you’ll likely have some symptoms – more on them below.
What Are Symptoms of High Blood Sugar?
Apart from testing, how do you know whether you have high blood sugar levels? Here are some symptoms that can indicate higher than normal blood sugar levels (also called “Hyperglycemia”):
- Constant hunger (even after a full meal)
- Constant thirst
- Frequent urination
- Fatigue after eating
- Blurry vision
- Difficulty concentrating
- Stubborn belly fat
This isn’t just a hunger or weight loss issue. When you have chronically high blood sugar levels, it can really mess up your hormones. But you can also be dealing with low blood sugar levels.
What Does it Mean to Have Low Blood Sugar?
Low blood sugar, or hypoglycemia, is another imbalance you could be dealing with. According to the National Institutes of Health, hypoglycemia is:
“defined by a plasma glucose concentration below 70 mg/dL; however, signs and symptoms may not occur until plasma glucose concentrations drop below 55 mg/dL.” (2)
People get hypoglycemia from eating a diet high in sugar and processed carbohydrates, whether that’s white sugar or flour, cookies, donuts, fruit juice, rice crackers, quinoa puffs, or even some protein powders.
After eating a meal containing such foods, blood sugar levels first go up and then they drop below optimal, manifesting in symptoms listed below.
Chronic hypoglycemia leads to pre-diabetes and eventually, diabetes. It’s important to get a handle on your blood sugar levels early on so that the imbalance doesn’t progress to the point of diabetes.
What Are Symptoms of Low Blood Sugar?
Here are some symptoms that can indicate lower than normal blood sugar levels (also called “hypoglycemia”):
- Having to eat every few hours to avoid crashing
- Needing sugar to “bring sugar levels up” two hours after eating
- When hungry, feeling/experiencing:
- Shakiness, nervousness, or anxiety
- Moodiness and lack of focus
- Sweaty; chills; clamminess
- Irritability or impatience
- Confusion, disorientation, even delirium
- Rapid or fast heartbeat
- Light-headiness or dizziness
Low blood sugar can be followed by high blood sugar after refueling, and then return to low blood sugar again. It’s a rollercoaster you don’t want to be on.
How Does Imbalanced Blood Sugar Impact Hormones?
Getting blood sugar levels under control is a key element to getting your hormones back to balanced. Here are a few ways that high blood sugar impacts hormones:
High Testosterone
High blood sugar is the main cause of high testosterone in women. That’s because high blood sugar levels suppress the production of sex hormone binding globulin (SHBG), which is supposed to bind excess sex hormones. Poor liver function can also lead to low SHBG. (3)
If you don’t have enough SHBG over time, you could end up developing the high testosterone condition of Polycystic Ovarian Syndrome (PCOS). This is a situation of cysts growing on your ovaries. Women who have PCOS often have the following symptoms:
- Irregular or no periods
- Stubborn belly fat
- Excessive facial hair
- Can’t get pregnant
- Super oily hair and skin (often leading to acne)
- Frontal balding
These are not fun symptoms to deal with. They can be debilitating, making it hard to get pregnant, lose weight and feel 100% our healthy selves. You can learn more about PCOS by reading these two articles:
If you’re wondering whether you may have PCOS, take our Hormone Quiz.
High blood sugar can cause high testosterone, but it can also cause higher than normal estrogen, leading to Estrogen Dominance.
Estrogen Dominance
I’ve talked about Estrogen Dominance many times on this website and it’s also the focus of my latest book, Overcoming Estrogen Dominance. Estrogen Dominance is when you have too much estrogen in circulation that is not balanced by progesterone. It can also be a circumstance of too much of “dirty” estrogens which are poorly metabolized estrogens.
Estrogen can get out of control as a result of too much testosterone. If your blood sugar is too high, leading to excess testosterone, your body can convert the testosterone into estrogen. It’s another way you can develop Estrogen Dominance.
Learn more about Estrogen Dominance here and find out where you fall on the estrogenic scale with our FREE assessment.
Adrenal fatigue
The adrenal glands have many different roles, but one of them is to stabilize blood sugar levels. If you keep spiking your blood sugar by eating a high sugar diet, your adrenal glands will have to work extra hard. Eventually, this could lead to adrenal dysregulation. It’s the same thing with low blood sugar levels. If you keep having periods of low blood sugar, it puts pressure on the adrenals as they keep having to boost your levels to stay in balance.
Insulin Resistance
Insulin resistance is a condition that happens when insulin is no longer moving sugar from the bloodstream to the muscle cells and fat cells like it’s supposed to. Then the sugar (glucose) levels in the blood stay high. The body becomes “resistant” to the effects of insulin. This situation is associated with metabolic syndrome and diabetes.
Metabolic syndrome is defined and diagnosed by certain group of symptoms and cardiovascular risk factors:
- Abdominal obesity/higher waist circumference/belly fat
- Dysregulated cholesterol with high LDL and low HDL
- High blood pressure
- Chronic inflammation
- Insulin resistance
- High blood sugar levels
All of these are linked to higher risk of developing conditions like type 2 diabetes and cardiovascular disease. (4)
Leptin Resistance
Chronically high blood sugar levels can also cause high leptin levels, and eventually lead to leptin resistance. (5) Leptin is a satiating hormone. Its opposite is ghrelin, the appetite hormone. Leptin Resistance is a similar situation to Insulin Resistance. It’s when leptin hormone levels are high for too long, and the brain starts to ignore it by shutting down its leptin receptors. If you have leptin resistance, you may find that you just can’t stop eating and never really feel satisfied.
Leptin is produced by fat cells, so the more fat you have, the more leptin you’ll have. When there’s so much leptin floating around, the body just starts to tune out. The leptin is there sending the message to the brain to stop eating, but since the leptin receptors in the brain have shut down, the message isn’t received. That’s how women have difficulty losing weight. The leptin produced by the fat cells just keeps telling them to keep eating.
Thyroid issues (Low or High)
Blood sugar ups and downs will also tend to inhibit thyroid function. Plus, if you’re feeding a candida overgrowth with sugar, you could be inhibiting the conversion of T4 hormone to the active T3.
In general, thyroid disorders are associated with insulin resistance and metabolic syndrome, which tend to be caused by chronically high blood sugar levels. (6)
This study showed a connection between subclinical (mild) hypothyroidism and insulin resistance. (7) A large study of over 8000 participants confirmed the hypothyroid-insulin resistance connection. (8)
You may find that you have several of these things going on at once. Can you do anything about it? Yes. We’ll start by talking about the impact of diet.
Diet For Supporting Balanced Blood Sugar Levels
There’s so much you can do with diet – hence, my first book, Cooking For Hormone Balance. Blood sugar balancing is very much dependent on what you eat throughout the day, starting with breakfast.
Start With a Truly Balanced Breakfast
A diet that supports balanced blood sugar starts the day in balance. You don’t want to start out the day with a blood sugar spike, or it will be downhill from there. Many women start the day with a high sugar breakfast and then wonder what happened, come 10am.
That’s probably where the 10am coffee and donut break came from!
Skip the donuts and coffee and instead start your day with what I call a PFF breakfast. PFF stands for Protein, Fat and Fiber. One of my personal favorite PFF breakfasts is the Farmer’s Wife Sunday Breakfast. You can read more about PFF Breakfasts and get some ideas here.
You can see how to make the Farmer’s Wife Sunday Breakfast here in this video:
Want more healthy, simple and nutritious breakfast ideas? Download our FREE 15 Breakfasts to Rebalance Your Hormones guide here.
Try Fermented (Pu’er) Tea
Try adding a Pu’er tea to your day. An animal study published in a 2015 issue of Food & Function discovered that the polysaccharides from Pu’er tea were better at stabilizing blood sugar than the anti-diabetic drug, Acarbose. (9)
With tea, you get side benefits, rather than the negative side effects of medication.
A review of animal studies published in 2018 also found that pu-erh tea could be helpful in lowering fasting blood sugar levels. Three weeks of daily tea consumption was necessary to get the full benefits. (10)
Pique Tea is one of my favorite tea companies. Their Pu’er tea is filled with gut-feeding probiotics, wild harvested from 250 year old tea trees, sugar-free and with no artificial sweeteners.
Find a Good Food Guide
If you’re looking for a step-by-step guide for getting your blood sugar levels under control, check out my book, Overcoming Estrogen Dominance. It includes a 14-day meal plan for two, which includes Breakfast, Lunch, and Dinner, plus morning and bedtime rituals.
Lifestyle to Support Blood Sugar

Stay Hydrated
Staying hydrated is important for maintaining balanced blood sugar. According to an observational study, those who drank more water overall tended to have lower blood sugar levels. (11)
Exercise and movement
Getting regular exercise may also help keep your blood sugar in balance — particularly by increasing insulin sensitivity. (12)
According to the American Diabetes Association, exercise lowers blood sugar by helping insulin take up glucose both during and after physical activity. Plus, it helps muscle cells directly take up glucose whether or not insulin is present. Regular exercise can also help lower your hemoglobin A1C. (13)
Additionally, lowering belly fat can help you get high blood sugar levels back under control. This absolutely does not mean you have to start jogging or running. Walking or strength training may be all you need.
A small study of 20 obese women in Korea found that those who walked for 50-70 minutes, 3 times a week for 12 weeks, reduced their waist circumference by an average of 1.1 inches. (14)
Two review studies reinforced that aerobic exercise like walking was helpful for reducing waist circumference, which is a part of metabolic syndrome and blood sugar dysregulation. (15, 16)
Strength training is often recommended for pre- and diabetics. A paper published in Current Sports Medicine Reports highlighted some benefits of strength training, which included lowering HbA1C (a marker of diabetes), reducing belly fat, and improving insulin sensitivity, as well as improving BMD. (17)
In a review published in 2020, researchers stated that a single bout of exercise could improve insulin sensitivity for up to 16 hours afterwards. (18)
Get Sleep
Getting adequate sleep is vital for maintaining normal blood sugar levels and appetite. Sleep deprivation increases the stress hormone cortisol in the evening hours, which then increases blood sugar levels. (19)
According to research published in the Annuls of the New York Academy of Sciences, sleep deprivation was associated with blood sugar dysregulation, decreased insulin sensitivity, and an increased risk for diabetes. (20)
Very much connected with getting enough sleep is managing your stress levels.
Manage Your Stress
Higher long-term stress levels can absolutely raise your blood sugar levels. Studies of diabetics have shown that the stress hormone, cortisol, when it stays high, can level to higher fasting blood sugar levels. (21)
There’s even a term called “Stress Hyperglycemia” that occurs at critical illness or infection. (22, 23)
Don’t brush off stress. Find things that help reduce your stress to help keep your blood sugar and hormones in balance. That could be something like yoga (24) or mindfulness type therapies (25) or whatever works for you.
Herbs and Supplements to Support Balanced Blood Sugar
There are some supplements that can support you as you work to get your blood sugar back into balance.
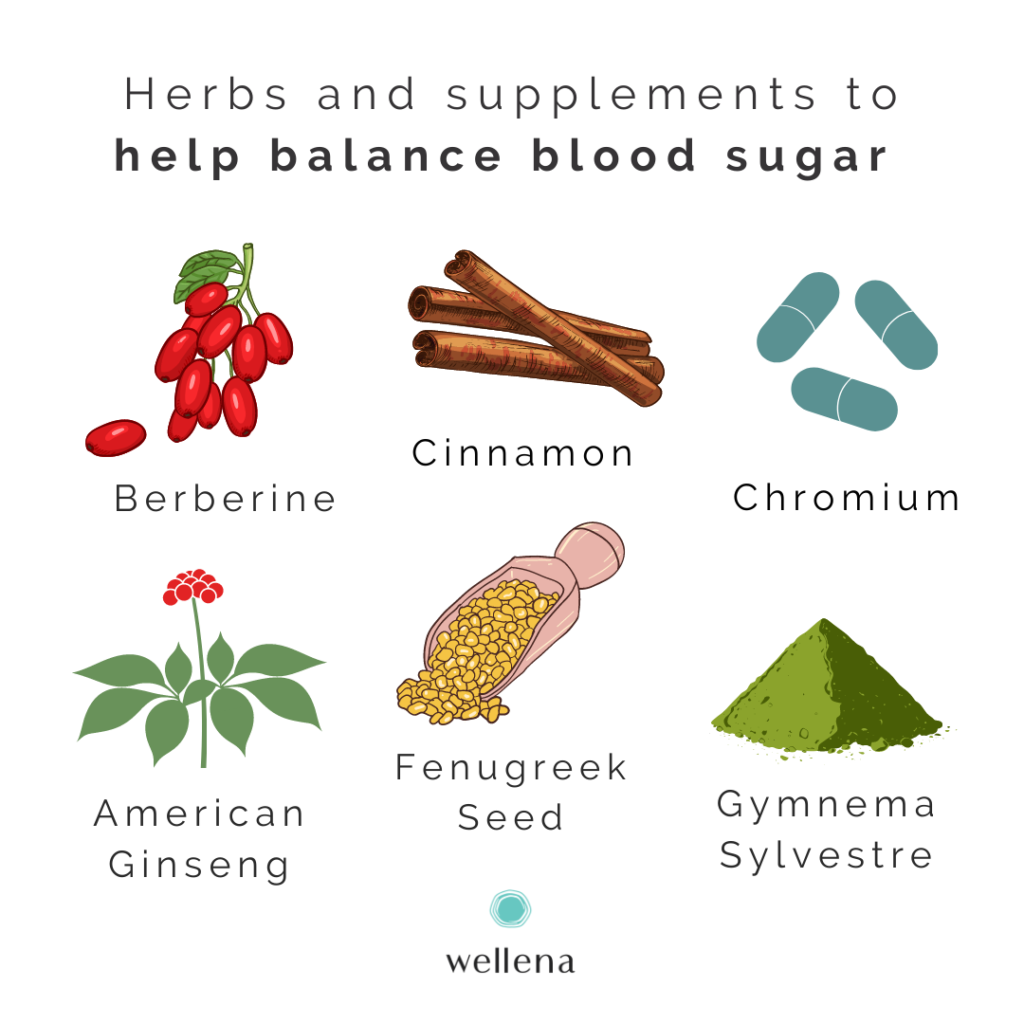
Here’s a short list of things to look for and how they help:
Berberine
Berberine is a compound present in a few different herbs, including barberry and Oregon grape (Mahonia aquifolium). In a review study, adding berberine supplements to diet and lifestyle changes, was helpful in improving fasting blood sugar and A1C, compared to diet and lifestyle with no supplement or with a placebo. (26)
In another study, berberine was found to improve insulin sensitivity and to help sugar go from the bloodstream to the muscle cells, which then lowered blood sugar. (27)
It’s important to note that berberine should only be used short-term (no longer than 8 weeks), and combined with a good diet.
Fenugreek
Fenugreek (Trigonella foenum graecum) is an herb that can help regulate blood sugar and insulin. It can also lower LDL cholesterol.
In a study of insulin-dependent (Type 1) diabetic patients, 100 grams of fenugreek seed powder was given during both the noontime and evening meals for 10 days. The fenugreek lowered fasting blood sugar, improved the results of the glucose tolerance test, and improved cholesterol and triglyceride numbers. (28)
In a study of 25 patients with newly diagnosed type 2 diabetes, a fenugreek seed alcohol extract improved their insulin sensitivity at a dosage of 1 gram per day over a 2 month time period. (29)
My Cooking for Hormone Balance cookbook has a Sugar Balancer Tea recipe that includes fenugreek.
American Ginseng
American Ginseng (Panax quinquefolius) was given as an “add on therapy” to patients with type 2 diabetes. The herbal extract (or a placebo) was given at a dosage of 1 gram with each meal (3 grams per day) for 8 weeks. Then, after a 4-week break, the placebo and ginseng were swapped for another 8 weeks (cross-over study). At the end of the study, researchers found that the American Ginseng significantly reduced hemoglobin A1C levels compared to the placebo. Fasting blood sugar also went down by nearly 10%. (30)
In a study of healthy people, American ginseng, at doses of 1-3 grams 40 minutes before meals, was helpful in reducing post-meal blood sugar levels. (31)
The way American ginseng works is as an insulin sensitizer, improving your body’s response to insulin. (32)
Gymnema Sylvestre
Another natural insulin sensitizer is an Ayuvedic herb, Gymnema Sylvestre. The Hindi name of the plant is “gurmar” which means “sugar destroyer.” (33)
Gymnema leaf is a powerful herb for controlling high blood sugar levels. It’s been used for thousands of years in the Ayurvedic and folk medicines of India to treat diabetes, malaria, and many other conditions. (34)
In a study of people with type 2 diabetes, gymnema leaf extract was given daily over 18 to 20 months. The 400 mg dose resulted in a 29% decrease in their fasting blood sugar levels. Hemoglobin A1C levels also went from 11.9% down to 8.48% by the end of the study and 5 out of the 22 patients were able to get off their medication and manage their diabetes with the gymnema extract alone. (35)
Cinnamon
Cinnamon is a great spice to add if you’re wanting to lower your blood sugar. According to a study published in the Journal of the American College of Nutrition, a component of cinnamon seems to imitate insulin, helping the body move sugar from the bloodstream into the cells. (36)
A review study involving 543 people with type 2 diabetes showed that cinnamon decreased fasting blood sugar levels by an average of about 24 mg/dL. (37)
Cinnamon is an easy way to add a blood-sugar balancing spice to your meals. You can even add it to your favorite hormone-balancing beverage.
Chromium
A deficiency in this mineral makes it harder for you to use carbohydrates for energy. (38)
A review published in the Journal of Clinical Pharmacy and Therapeutics found that chromium of a dose of 200 micrograms a day improved hemoglobin A1C and fasting blood sugar levels, compared to a placebo. (39)
The best form for absorption seems to be Chromium picolinate. (39)
ONE Supplement You Can Add
If you’re feeling overwhelmed with all the different supplement options, and just want one go-to supplement, we’ve got you covered. Wellena’s Gluco Maximus supplement was formulated with the following herbs:
- Green Tea Extract
- American Ginseng
- Gymnema Extract
- Cinnamon
Plus, it also includes Alpha Lipoic Acid (ALA) and Chromium for extra blood sugar support. This supplement is non-GMO, gluten-free, dairy-free, soy-free, yeast-free, sugar-free, and colorant-free.
If you also want to tackle chronic inflammation and depleted minerals, we’ve put together a kit for you. It’s called the Sugar Balance Protocol.
The Sugar Balance Kit includes:
- Gluco Maximus just mentioned
- Curcumina
These 2 supplements work together to support blood sugar balance, mineral balance, and a proper inflammatory response. When you purchase both supplements together in this kit, you save $12.80.
To learn more about blood sugar balancing and hot flashes, check out this article.
Resources
- Mouri, MI and Badireddy, M. Hyperglycemia. StatPearls [Internet]. January 2021. [Updated May 10, 2021].
- Mathew, P. and Thoppil, D. Hypoglycemia. StatPearls [Internet]. January 2021. [Updated May 10, 2021].
- Strain, G et al. “The relationship between serum levels of insulin and sex hormone-binding globulin in men: the effect of weight loss.” The Journal of clinical endocrinology and metabolism. 1994.
- Bovolini, António et al. “Metabolic Syndrome Pathophysiology and Predisposing Factors.” International journal of sports medicine. 2021.
- Kennedy JIC, Askelund KJ, Premkumar R, et al. Leptin Is Associated With Persistence of Hyperglycemia in Acute Pancreatitis: A Prospective Clinical Study. Medicine. 2016
- Kapadia, Kunal B et al. “Association between altered thyroid state and insulin resistance.” Journal of pharmacology & pharmacotherapeutics. 2012.
- Vyakaranam, Sapna et al. “Study of Insulin Resistance in Subclinical Hypothyroidism.” International journal of health sciences and research. 2014.
- Chaker, Layal et al. “Thyroid function and risk of type 2 diabetes: a population-based prospective cohort study.” BMC medicine. Sep. 2016.
- Deng, Yea-Tyz et al. “Pu-erh tea polysaccharides decrease blood sugar by inhibition of α-glucosidase activity in vitro and in mice.” Food & function. 2015.
- Lin, H.-C., Lee, C.-T., Yen, Y.-Y., Chu, C.-L., Hsieh, Y.-P., Yang, C.-S. and Lan, S.-J. Systematic review and meta-analysis of anti-hyperglycaemic effects of Pu-erh tea. International Journal of Food Science + Technology. 2019.
- Roussel, Ronan et al. “Low water intake and risk for new-onset hyperglycemia.” Diabetes care. 2011.
- Borghouts, L B, and H A Keizer. “Exercise and insulin sensitivity: a review.” International journal of sports medicine. 2000.
- American Diabetes Association. Blood Sugar and Exercise. 2021.
- Hong, Hye-Ryun et al. “Effect of walking exercise on abdominal fat, insulin resistance and serum cytokines in obese women.” Journal of exercise nutrition & biochemistry. 2014.
- Ismail, I et al. “A systematic review and meta-analysis of the effect of aerobic vs. resistance exercise training on visceral fat.” Obesity reviews : an official journal of the International Association for the Study of Obesity. 2012.
- Ohkawara, K et al. “A dose-response relation between aerobic exercise and visceral fat reduction: systematic review of clinical trials.” International journal of obesity. 2005.
- Westcott, Wayne L. “Resistance training is medicine: effects of strength training on health.” Current sports medicine reports. 2012.
- Borghouts, L B, and H A Keizer. “Exercise and insulin sensitivity: a review.” International journal of sports medicine. 2000.
- Leproult, Rachel, and Eve Van Cauter. “Role of sleep and sleep loss in hormonal release and metabolism.” Endocrine development. 2010.
- Knutson, Kristen L, and Eve Van Cauter. “Associations between sleep loss and increased risk of obesity and diabetes.” Annals of the New York Academy of Sciences. 2008.
- Pena Dias, J., et al. The longitudinal association of changes in diurnal cortisol features with fasting glucose: MESA. Psychoneuroendocrinology. 2020.
- Ali Abdelhamid, Yasmine et al. “Stress hyperglycaemia in critically ill patients and the subsequent risk of diabetes: a systematic review and meta-analysis.” Critical care (London, England). September, 2016.
- Magee, Matthew J et al. “Stress Hyperglycemia in Patients with Tuberculosis Disease: Epidemiology and Clinical Implications.” Current diabetes reports. Aug. 2018.
- Sahay, B K. “Role of yoga in diabetes.” The Journal of the Association of Physicians of India. 2007.
- Hartmann, Mechthild et al. “Sustained effects of a mindfulness-based stress-reduction intervention in type 2 diabetic patients: design and first results of a randomized controlled trial (the Heidelberger Diabetes and Stress-study).” Diabetes care. 2012.
- Lan, Jiarong et al. “Meta-analysis of the effect and safety of berberine in the treatment of type 2 diabetes mellitus, hyperlipemia and hypertension.” Journal of ethnopharmacology. 2015.
- Yin, Jun et al. “Efficacy of berberine in patients with type 2 diabetes mellitus.” Metabolism: clinical and experimental. 2008.
- Sharma, R D et al. “Effect of fenugreek seeds on blood glucose and serum lipids in type I diabetes.” European journal of clinical nutrition. 1990.
- Gupta, A et al. “Effect of Trigonella foenum-graecum (fenugreek) seeds on glycaemic control and insulin resistance in type 2 diabetes mellitus: a double blind placebo controlled study.” The Journal of the Association of Physicians of India. 2001.
- Vuksan, Vladimir et al. “Efficacy and safety of American ginseng (Panax quinquefolius L.) extract on glycemic control and cardiovascular risk factors in individuals with type 2 diabetes: a double-blind, randomized, cross-over clinical trial.” European journal of nutrition. 2019.
- Vuksan, V et al. “American ginseng (Panax quinquefolius L.) attenuates postprandial glycemia in a time-dependent but not dose-dependent manner in healthy individuals.” The American journal of clinical nutrition. 2001.
- McKennon, Skye A. “Non-Pharmaceutical Intervention Options For Type 2 Diabetes: Diets And Dietary Supplements (Botanicals, Antioxidants, and Minerals).” Endotext. June, 2018.
- Shiyovich, Arthur et al. “Toxic hepatitis induced by Gymnema sylvestre, a natural remedy for type 2 diabetes mellitus.” The American journal of the medical sciences. 2010.
- Khan, Farzana et al. “Comprehensive Review on Phytochemicals, Pharmacological and Clinical Potentials of Gymnema sylvestre.” Frontiers in pharmacology. October, 2019.
- Baskaran, K et al. “Antidiabetic effect of a leaf extract from Gymnema sylvestre in non-insulin-dependent diabetes mellitus patients.” Journal of ethnopharmacology. 1990.
- Jarvill-Taylor, K J et al. “A hydroxychalcone derived from cinnamon functions as a mimetic for insulin in 3T3-L1 adipocytes.” Journal of the American College of Nutrition. 2001.
- Allen, Robert W et al. “Cinnamon use in type 2 diabetes: an updated systematic review and meta-analysis.” Annals of family medicine. 2013.
- National Institutes of Health: Office of Dietary Supplements. Chromium – Health Professional Fact Sheet. U. S. Department of Health and Human Services website. Updated March 2021.
- Suksomboon, N et al. “Systematic review and meta-analysis of the efficacy and safety of chromium supplementation in diabetes.” Journal of clinical pharmacy and therapeutics. 2014.

Can you take the Glucos Maximus for eight weeks only given there is berberine in it? You mentioned in a post about balancing blood sugar that berberine should not be taken for more than eight weeks.
Hi Roni, Yes the Glucos Maximus can be taken for up to 8 weeks while you work on diet and nutrition to help balance the underlaying issue. If blood sugars are still dysregulated at 8 weeks it is important to check with a good functional medicine practitioner to help guide you with further support. ~HB Team
Do you know of any good functional medicine practitioners who work with people remotely (online)? I live in an FM desert and for me the conventional doctors have nothing to offer. I wish there were a directory of FM practitioners who could work online with clients.
Hi Lumina, yes, there is a directory to look for someone that you resonate with. Here is a link for you. https://www.ifm.org/find-a-practitioner/ Best of luck! Jennifer @HB support
Just a few thoughts on the article.
My holistic nutritionist here in Canada, has got me eating every 4-5 hours maximum, in between meals . This is to help with balancing my blood sugar. I am 62. I was eating breakfast and dinner, maybe a snack in between. I wasn’t hungry. This change with eating more food and incorporating movement, I have managed to loose my stomach size one belt notch. Quantity, and timing, is just as important as quality in our food choices.