What You Will Learn in This Article
- Symptoms of Hot Flashes
- Triggers of Hot Flashes
- Potential Mechanisms/Causes
- Why Some Women Suffer More
- Solutions for Hot Flashes
Hot flashes are the bane of many a peri- or post-menopausal woman’s existence–especially since they are linked to insomnia and depression. While the mechanism of this irritating symptom isn’t fully understood, there are things that can be done to lessen both the frequency and the severity of hot flashes.
Before we get started, see if Estrogen Dominance is the root cause of your hot flashes with my free assessment.
What do Hot Flashes Feel Like?
Hot flashes tend to come on suddenly (hence, “flash”) and involve a number of distressing and uncomfortable symptoms:
- Sudden warmth of face, neck, and chest
- Sweating
- Increased pulse rate
- Chest tightness
- Anxiety
- Flushed skin, sometimes blotchy
- Sometimes followed by a chill
If it’s not enough to have these unpleasant mini sauna sessions during the day, they are often accompanied by night sweats that wake you from a pleasant slumber. This can lead to insomnia, sleep deprivation, and feelings of hopelessness and depression.
Hot Flash Triggers
The 5 most common reported triggers of hot flashes (2) are the following:
- Stress/Emotional situations (59%)
- External heat (44%)
- Confining space (38%)
- Alcohol (20%)
- Caffeine (17%)
Note, those triggers simply bring on a hot flash. They aren’t actual causes of the imbalance. I, therefore, looked deeper into what are the underlying causes of hot flashes.
7 Causes of Hot Flashes
While the mechanism isn’t completely understood, medical experts believe hot flashes originate in the brain and are caused by the dysregulation of the temperature control mechanism in the hypothalamus. Certain hormones/catecholamines, adrenaline (epinephrine), noradrenaline (norepinephrine), as well as thyroid hormone are likely involved.
Blood Sugar Imbalance
Essentially, what this means is that anything that puts stress on the brain and body can be a contributor to hot flashes. That includes blood sugar issues and hypoglycemia. Studies have found that a drop in blood sugar can trigger hot flashes (5).
When I was in private practice, I used to work with Dr. Francis who was an emergency physician. She used to experience debilitating hot flashes at exactly 11:00 a.m. each morning. The problem was that they would strike in the middle of her shift when she often was saving lives. Something had to change. After initial reluctance, she sent me her food journal, which said that her 8:00 a.m. breakfast consisted of cereal, topped with fruit and yogurt. She had also noted that if she had a handful of walnuts (full of protein, fat, and fiber!) around 10:45 a.m., she wouldn’t get a hot flash.
That was a great observation and one that proved that her dropping blood sugar level around 11:00 a.m. was the cause of her hot flashes. She wasn’t always able to snack to prevent a hot flash, and I wanted to focus on the bigger picture and prevent her blood sugar levels from dropping in the first place.
We changed her breakfast to a PFF (Protein, Fat, Fiber) kind of breakfast and her hot flashes immediately stopped. This is why most of the breakfast recipes in my books (including Overcoming Estrogen Dominance) are based on the PFF principle.
Dropping Estrogen Levels
It is no surprise that hot flashes are most common in aging women who enter peri- or menopause when their estrogen production starts dropping. The mechanism behind it isn’t fully understood but I believe that blood sugar balance and inflammation, when combined with dropping estrogen levels is the perfect storm.
Take my free assessment to learn more about Estrogen Dominance and if your symptoms are linked to this common hormonal imbalance.
Low Progesterone
Progesterone is also likely involved here. Estrogen can cause anxiety when out of balance with progesterone, as progesterone has an anti-anxiety effect on the body. As progesterone levels decline and fail to balance estrogen, the body is also put in more of a stressed, high adrenaline state.
Inflammation
Additionally, low grade systemic inflammation has been tied to hot flashes (11). What can cause chronic systemic inflammation? Certainly dietary choices–an inflammatory diet or eating foods that cause inflammation in an individual (especially food intolerances).
A study of postmenopausal women and diet (12) found that those who consumed a higher antioxidant diet had fewer hot flashes.
Many women in our Hormones Balance community have reported a reduction of hot flashes with a change of diet–especially after removing inflammatory foods such as gluten, dairy, reducing sugar and coffee (or completely cutting out all caffeine).
Mineral Deficiencies
Mineral deficiencies, such as magnesium (10), and possibly zinc and selenium may also contribute to hot flashes.
Ethnicity
A study of over 16,000 American women found that African Americans and Hispanics were more likely to experience hot flashes than other ethnic groups, including Caucasians (3). The distribution of women likely to have hot flashes was as follows:
- African American (46%)
- Hispanic (36%)
- Caucasians/Whites (31%)
- Chinese (21%)
- Japanese (18%)
Lifestyle factors: Smoking
Smoking is one of the few lifestyle factors that is consistently associated with hot flashes. Women who smoke are more likely to experience hot flashes than nonsmokers. In fact, over the course of 6 years, smokers had a 60% increased risk of vasomotor symptoms like hot flashes as compared to nonsmokers (4).
Even though hot flashes aren’t fully understood, there are still a number of things you can do to lessen the frequency or severity of hot flashes… or to eliminate them altogether.
Solutions for Hot Flashes
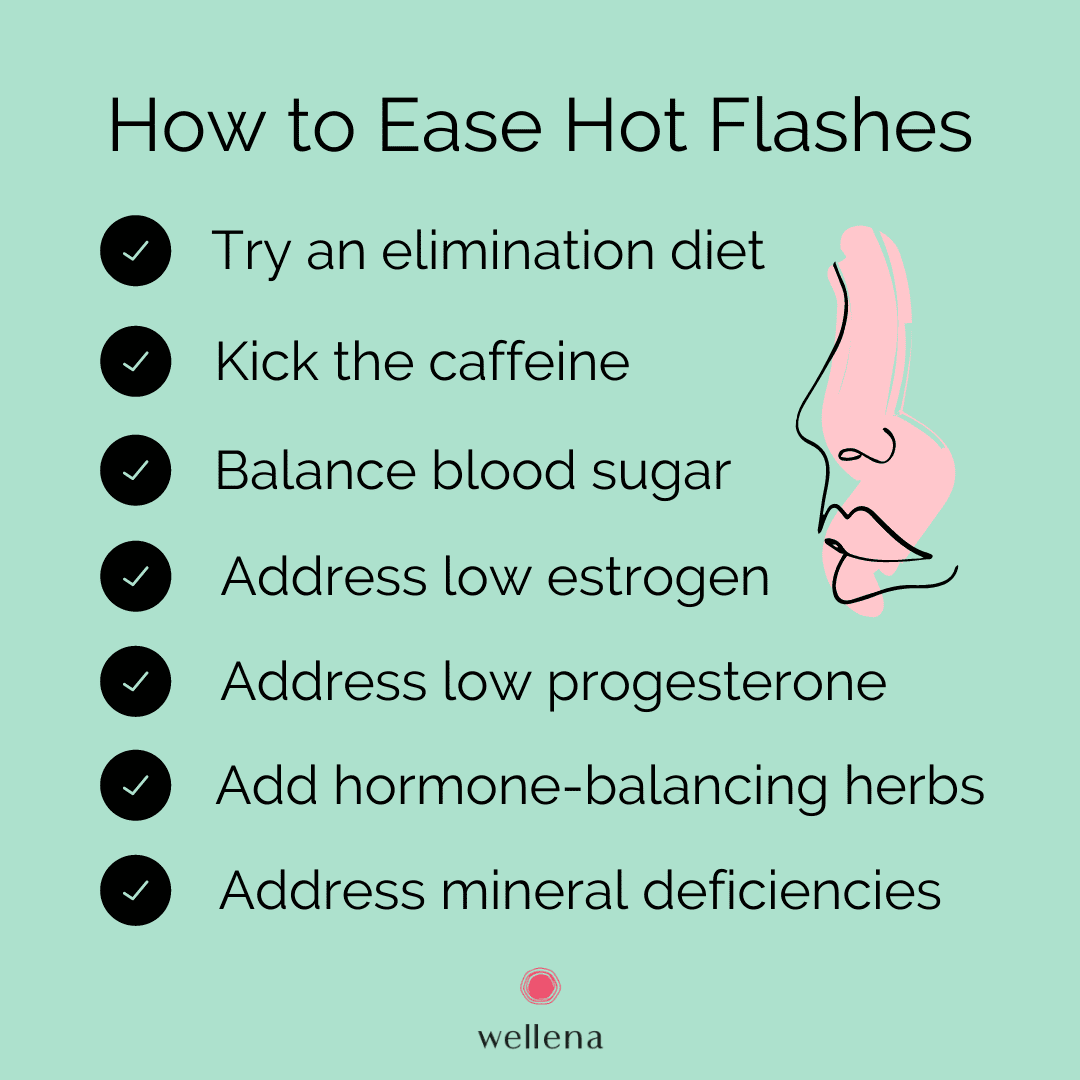
Diet (Elimination Diet)
Diet is really important here. Hot flashes are yet another sign of hormone imbalance, and my first-line therapy for balancing hormones has always been food. (Hence, the creation of my book, Overcoming Estrogen Dominance). Download my 15 breakfasts guide, filled with nutritious recipes to reduce or stop hot flashes in their tracks.
Here are some things to consider:
- Is your diet generally inflammatory or anti-inflammatory?
- Are you intolerant to some of the otherwise healthy foods you’re eating? Gluten and dairy are common culprits.
- Is your diet causing blood sugar dysregulation?
- If you answered “yes” to any of the above, you may want to consider trying an Elimination Diet.
Elimination Diet
An Elimination Diet, which removes potentially inflammatory or allergenic foods, may be the best way to start. There are many versions of this, such as Whole 30, the Paleo Diet, the Autoimmune Paleo Diet, the Wahls Protocol, the Virgin Diet, etc. Generally, the idea is to remove dairy, soy, gluten, corn, sugar, alcohol, and processed foods. Some versions may also remove eggs, nuts, nightshades, grains in general, legumes, and more.
An elimination diet at its most restrictive lasts only 4 to 6 weeks, and then the diet is expanded. If reactions occur after re-introducing a food, the person is most likely intolerant to that food. Healthy foods causing reactions are removed from the diet until health is improved and the immune system is more in balance.
Many of our program participants have said that after starting the Elimination Diet, their hot flashes disappeared.
Kick the Caffeine
When addressing hot flashes through diet, I hate to break it to you, but it’s really best to also remove coffee. Unfortunately, coffee contributes to estrogen dominance (13), and caffeine may increase blood sugar levels (14).
In my experience, many women who have given up coffee and caffeine report better sleep within days, fewer hot flashes, and other benefits over time.
Balance Blood Sugar
Unbalanced blood sugar levels can cause the body to stay stuck in an inflammatory state, leading to the overproduction of stress hormones and then a general state of hormone imbalance, including estrogen dominance. We know from studies that blood sugar problems (5) and inflammation can contribute to hot flashes (11).
In order to balance your blood sugar, I recommend starting your day with a PFF breakfast. PFF stands for Protein, Fat, and Fiber and is the first step in eating to promote balanced blood sugar levels. Get our free 15 breakfasts guide with delicious, fast and simple recipes to help balance your hormones.
Berberine, fenugreek, kudzu, banaba, and cinnamon are some of the plants and herbs renowned for up-regulating insulin receptors that help balance blood sugar levels. When you combine it with a low-sugar diet, your blood sugar levels are bound to stabilize quickly and you may kiss hot flashes goodbye. Our Wellena Gluco Maximum contains these herbs (and more) and have been a very popular product with our community.
Tip: If you’re experiencing symptoms Estrogen Dominance, you can find out more by taking my Free Estrogen assessment here.
Reduce Inflammation
When you implement all of the above suggestions, your inflammation levels are bound to come down. If you feel like you need additional help in lowering inflammation, try adding Inflammavail™ which is a supplement containing boswellia (frankincense) and turmeric as the hero ingredients; designed to help balance the body’s inflammatory response.
Address Low Progesterone
Low progesterone may also lead to hot flashes. Progesterone is a hormone that helps balance the effects of estrogen in the body. It’s very sensitive to stress in our lives. There are a number of nutrients that can help boost your progesterone naturally; however, for many women, a topical progesterone is a more efficient way to raise your progesterone to healthy levels. This study found that a form of progesterone reduced hot flashes by up to 80% (15).
ProgestPure, by Wellena, is a natural and clean topical progesterone serum providing 20 mg of bioidentical progesterone in each 1 ml dose. This highly bioavailable form of progesterone contains four ingredients: micronized USP progesterone, dimethyl isosorbide, Caprylic/capric triglyceride (from coconut), and vitamin E. It’s free of parabens, mineral oil, and petroleum. I use it personally (and won’t put out this product to our community if it wasn’t of the highest quality).
The progesterone used in ProgestPure is super-micronized and is delivered in a proprietary triglyceride carrier which helps the progesterone absorb more efficiently as compared to conventional creams. This serum also contains a natural sugar-based complex, dimethyl isosorbide, which increases progesterone solubility and helps the progesterone penetrate more deeply through the skin and at a faster rate.
Additionally, the dimethyl isosorbide helps preserve the potency of the progesterone after manufacturing. This is in contrast to water-based products, which can lose as much as 30% or more of its potency within the first 60-90 days after manufacturing.
Women going through perimenopause, menopause, and post-menopause and suffer from hot flashes can use topical progesterone for 25 days out of a 30-day calendar, with 5 days off. If you are in peri-menopause and still menstruating, start progesterone 5 to 7 days after the first day of your period and continue until the next period.
You can find our ProgestPure and try it for yourself here.
Address Low Estrogen
Low estrogen is another hormonal contributor to hot flashes. Flaxseed, with its high levels of phytoestrogens is a great natural way to increase estrogen. A review of 62 studies using plant-based therapies for menopause symptoms in 6653 women found that phytoestrogens, such as those found in flax, helped reduce hot flashes.
You can also try adding reishi mushrooms, which were shown (16) to be able to naturally regulate low estrogen levels that were associated with menopause.
Address Mineral Deficiencies
Mineral deficiencies may also contribute to hot flashes.
Try adding magnesium in the form of magnesium glycinate. A small 2011 study of 29 women published in the journal, Supportive Care in Cancer, found that supplementing with 400 to 800 mg of magnesium per day helped reduce the frequency and intensity of their hot flashes over a 4 week period. The study used Magnesium oxide, which I don’t recommend, due to its low bioavailability (only 4%). The highly bioavailable Magnesium glycinate is a much better bet.
In Summary
Remember: Take away before you add. Remove the high carb, inflammatory, glucose-spiking foods. Remove foods you are sensitive to. Lower stress and inflammation. Add in colorful whole foods as you start Overcoming Estrogen Dominance. Try balancing your hormones with quality supplements (we hold all of our Wellena supplements to the highest standards). Don’t stress about all the options. Relax and practice gratitude for each day.
As you become more balanced, your hypothalamus and thermostat will balance, too. Download our 15 free breakfasts to help.
Resources
- Hays, Bethany. Female Hormones: The Dance of the Hormones, Part I. The Textbook of Functional Medicine. 2010.
- Ziv-Gal, A. et al. Factors that may influence the experience of hot flushes by healthy middle-aged women. Journal of Women’s Health. 2010.
- Gold, E.B. et al. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40–55 years of age. American Journal of Epidemiology. 2000.
- Thurston, R. C. and Joffe, H. Vasomotor symptoms and menopause: findings from the Study of Women’s Health across the Nation. Obstetrics and Gynecology Clinics of North America. 2011.
- Dormire, Sharon and Howharn, Chularat. The effect of dietary intake on hot flashes in menopausal women. Journal of Obstetric, Gynecologic, and Neonatal Nursing. May/June, 2007.
- Mayo Clinic Staff. Hot flashes. Mayo Clinic website. 2018.
- Smith, Rebecca L. et al. Factors Associated with Poor Sleep During Menopause: Results from the Midlife Women’s Health Study. Sleep Medicine. 2018.
- Zeleke, B. M., et al. Vasomotor symptoms are associated with depressive symptoms in community-dwelling older women.
Menopause. June, 2017. - Franco, Oscar H. et al. Use of plant-based therapies and menopausal symptoms: a review and meta-analysis. JAMA. June 2016.
- Park, H. et al. A pilot phase II trial of magnesium supplements to reduce menopausal hot flashes in breast cancer patients. Supportive Care in Cancer. 2011.
- Huang, Wan-Yu et al. Circulating interleukin-8 and tumor necrosis factor-α are associated with hot flashes in healthy postmenopausal women. PLOS one. August, 2017.
- Abshirini, M. et al. Dietary total antioxidant capacity is inversely related to menopausal symptoms: a cross-sectional study among Iranian postmenopausal women. Applied Nutritional Investigation. March, 2018.
- Lam, Michael. The Role of Adrenal Fatigue in Estrogen Hormone Dominance. DrLamCoaching.com. Accessed February 24, 2020.
- Pizziol, A. et al. Effects of caffeine on glucose tolerance: a placebo-controlled study. European Journal of Clinical Nutrition. November, 1998.
- Shanafelt, T. D. et al. Pathophysiology and Treatment of Hot Flashes. Mayo Clinic Proceedings. November, 2002.
- Shimizu, K. Estrogen-like activity of ethanol extract of Ganoderma lucidum. Journal of Wood Sciences. 2009.
- Feature photo by Trent Szmolnik
Great article, thanks. At present, the onset of menopause often coincides with a woman reaching a certain standard of living – the prevailing family environment, career success, and high self-esteem. And hormonal changes disrupt the usual course of things, affecting well-being and attitude. Before modern medicines appeared on the shelves of pharmacies, many preferred steadfastly to endure all the symptoms of the extinction of reproductive function. Others – resorted to the help of folk remedies, often ineffective and even dangerous. But now there is no need for such extremes because reducing to a minimum of discomfort after menopause is possible with the help of modern medicines. Good luck!
I (72 year-old woman) ave been on biodentical hormones through a “specialist” ; unfortunately, the cost & distance of the provider & a new inexpensive all-in-one pill format called Bijuva, plus some other supplements (I think) got me to have hot flashes when I never had before! Now off them & trying to get straightened out. Problem is a very substantial absence of knowledgeable & affordable people in this field, particularly in rural Minnesota😩
Hey Chally,
Many clients have had success with a functional medicine doctor. If you need help locating one in your area, here is a good tool:
https://www.ifm.org/find-a-practitioner/
Also, please feel free to reach out to us at [email protected].
Healthy Regards,
HB team