What You Will Learn in This Article
- Who gets belly fat?
- The difference between visceral and other fat
- Risks associated with visceral fat
- Belly fat and insulin resistance
- How insulin resistance wrecks your hormones
- How do you know if you’re insulin resistant?
- Belly fat solutions
Belly fat is probably one of the most frustrating health and beauty issues a woman going into peri- and menopause can face.
We like having curves, but not that kind. The strange thing about belly fat is that you can lose twenty pounds and be slender everywhere else… and yet the belly fat remains. Or, you’ve been slim your whole life and suddenly this belly won’t go away. What’s the deal? Why is belly fat so difficult to get rid of -even if our other fat melts away?
The thing is, belly fat isn’t just fat. It indicates there’s a deeper imbalance going on. Is it related to hormone imbalance? Absolutely. Let’s dive in.
Who Gets Belly Fat?
Belly fat most often appears in women after the age of 45. It suddenly appears out of nowhere – even in skinny and athletic women, and it tends to worsen after 50. That is unless you make some diet and lifestyle changes. While the timing has a lot to do with the hormone changes accompanying perimenopause and menopause, it’s not a given.
Women who get belly fat tend to display some level of insulin resistance (IR), which we’ll talk about later on in this article. You may feel like it’s not you but keep reading as you don’t need to be a diabetic to develop insulin resistance.
The Difference Between Visceral and Other Fat
There are two main types of belly fat: visceral fat and subcutaneous (below the skin) fat. Subcutaneous fat is the fat just below the skin – the fat you can grasp with your hand. Visceral fat is deeper in your body. It gets its name from the fact that it surrounds the viscera – the organs in the abdominal cavity. (1)
There’s a vast difference between visceral and other body fat. It’s not just a vanity issue; belly fat becomes an endocrine organ that releases hormones. It also releases pro-inflammatory cytokines, sending waves of inflammation throughout the body.
Risks Associated With Visceral Fat
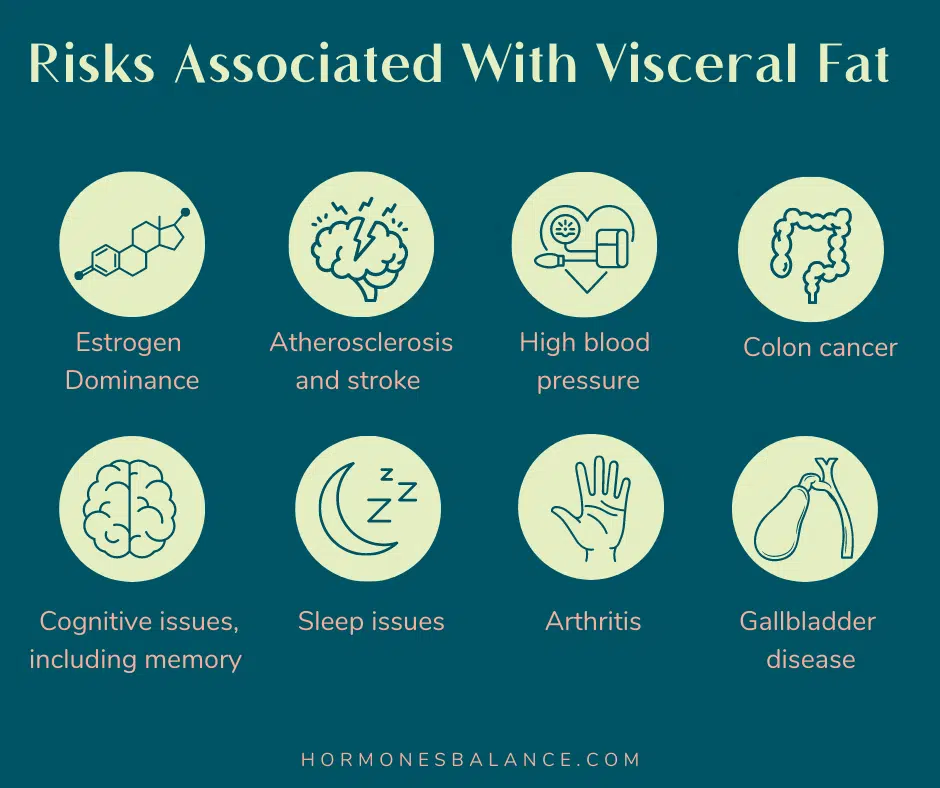
Visceral fat has a lot of health risks associated with it. Some associations researchers have made include:
- Estrogen dominance (visceral fat releases estrogen)
- Atherosclerosis and stroke
- High blood pressure
- Colon cancer
- Cognitive issues, including memory
- Sleep issues
- Arthritis
- Gallbladder disease
In women, belly fat is also associated with breast cancer and gallbladder disease.
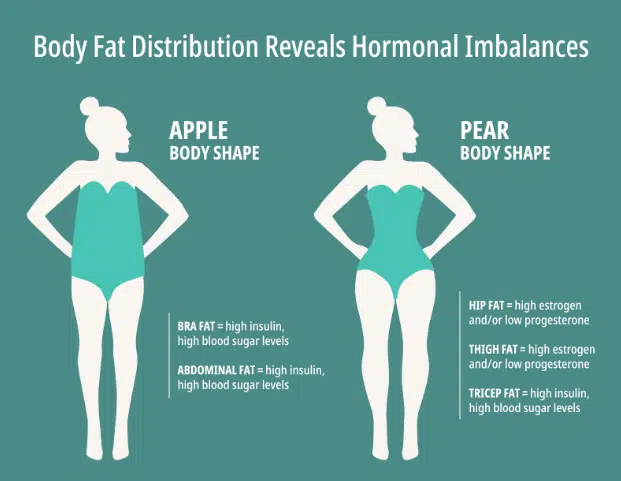
See the illustration of the apple-shaped woman versus the pear-shaped woman? The pear-shaped woman, even if she has some extra around the hips, tends to be in a healthier place hormonally than the apple-shaped woman. She’s at less risk for insulin resistance and the health problems that go along with it. That’s because the apple shape reflects insulin resistance. (1)

Belly Fat and Insulin Resistance
Belly fat is a classic sign of some level of insulin resistance. Insulin is a hormone made by the pancreas that helps blood sugar (glucose) get from your bloodstream into your cells as energy – insulin is like a key that opens the cell’s door to let glucose in.
Insulin resistance happens when the cells stop responding to the insulin at normal levels – the doors get shut and the key no longer works. As a result, the body makes more insulin, but cells may still resist the insulin message, now causing both high insulin and high blood sugar.
Cause #1: Sugar and Processed Carbs
One cause of insulin resistance is simply overeating sugar and processed carbohydrates over time. The insulin receptors on the cells just get worn out from trying to get all that glucose out of the bloodstream and into the cells. Eventually, they stop responding. This is a common occurrence in the American population. In fact, about 30% of Americans currently suffer from it. That explains why belly fat is so common these days. (2)
Cause #2: Aging and Reduced Insulin Response
Another cause of insulin resistance is aging. As we age, our insulin sensitivity gradually decreases. Blood sugar dysregulation also gets worse. A National Health and Nutrition Examination Survey published in Diabetes Care found that in the United States, 20.9% of those in their 20s and 30s had blood sugar issues. It was 46.9% of those in their 40s and 50s, 67.4% in those in their 60s through age 74, and 75.6% in those 75 or older. (3)
That’s why losing fat around the middle gets harder as you age. It also means you’re less tolerant of sugar as you approach peri-menopause and after.
Cause #3: Prescription medications
A third potential cause of insulin resistance is medication. Several types of cancer therapeutics may cause insulin resistance, including chemotherapy, steroids, hormone therapies, and other targeted drugs. (4) Other medications that may lead to insulin resistance and diabetes include thiazide diuretics (used for high blood pressure), beta-blockers (for high blood pressure, glaucoma, and heart disease), statins (for cholesterol and heart disease), antipsychotics, antidepressants, and more. (5)
How Insulin Resistance Wrecks Your Hormones
Insulin is a hormone. It’s part of the endocrine system. So, you better believe that it impacts the other hormones. High insulin levels cause the conversion of testosterone into excessive estradiol by an enzyme called aromatase. This promotes estrogen dominance. (2)
It becomes a vicious cycle because estrogen dominance makes insulin receptors less accepting of insulin, worsening insulin resistance.
How High Fatty Acids Which Hormone is Determine Released
Belly fat secretes free fatty acids that flow into the liver and circulate in the body. Too many fatty acids in the liver mean that the liver has to produce too much glucose, raising blood sugar and contributing to insulin resistance.
High circulating free fatty acids causes an increase in androgens like testosterone. This can lead to conditions like Polycystic Ovarian Syndrome (PCOS). It also induces serine phosphorylation of a particular enzyme (p450c17) which ultimately determines whether the steroid-making process ends up releasing cortisol or sex hormones. (6)
How Do You Know If You’re Insulin Resistant?
There are two ways to know whether or not you’re insulin resistant: Symptoms and labs. Your symptoms may give you an idea it’s time to get some labs drawn.
Symptoms of Insulin Resistance
There are some pretty clear symptoms of insulin resistance. Here’s what to look for: (2)
- Belly fat (apple shape)
- Skin tags around the neck and head area
- Elevated blood pressure (135/85)
- Hunger after eating a meal
- Tiredness after eating a meal
- Daytime drowsiness/fatigue
- Insomnia
- Cravings for sugar and processed carbohydrates
- Weight gain around the middle
- Frequent illnesses
Labs for Insulin Resistance
There are a few different lab tests you can ask for to find out whether you’re insulin resistant: (2)
- Fasting Blood Glucose (above 90 indicates IR)
- Fasting Insulin (above 15 indicates IR)
- Hemoglobin A1C (a result over 5.4 indicates IR)
- Homocysteine (a result over 30 indicates IR)
- HDL (a result less than 40 may indicate IR)
- Triglycerides (a result over 150 may indicate IR)
Belly Fat Solutions
You don’t need to starve yourself or go under the knife to get rid of belly fat. There are several things you can do to gradually slim down:
Lifestyle
Lifestyle is superior to drugs when it comes to losing belly fat. In a study published in the journal Circulation, scientists divided 3200 adults with blood sugar dysregulation into three groups. One group got the traditional drug, Metformin, one group exercised 150 minutes per week with a brisk walk (lifestyle change), and one group just got the usual care.
At a three-year follow-up, participants in both the lifestyle group and the drug group had reduced their progression toward diabetes. However, in the lifestyle group, it was 58%, while in the drug group, it was 31%. (7)
It’s encouraging that exercise can be more effective than medications. However, please don’t start running! Keep reading, as we’ll share recommendations later in the article.
Reduce Inflammation
Inflammation is the common thread that ties all chronic diseases and conditions together. As long as inflammation remains high, the body is in an emergency state and not in a healing state. That’s why reducing inflammation has to come first.
How do you reduce inflammation? By taking away the things contributing to inflammation and adding the things that help the body get back into homeostasis (balance).
That means focusing on things like:
- Diet – Low sugar, whole food diet, avoid foods you’re sensitive to (this includes inflammatory foods such as gluten, dairy, corn, eggs, and soy).
- Sleep – Aim for 8 hours a night, and be in bed before 10 pm.
- Exercise – weight lifting (not cardio) to increase insulin sensitivity.
- A positive outlook – Expect good things and practice gratitude.
Diet plays a key role in this, and you may have to go beyond a generally healthy diet if you want to lose fat.
Diet
Diet is a vital weapon in the battle of the bulge, particularly because of food’s effects on inflammation. To get a handle on your inflammation levels, the best place to start is an Elimination Diet. You can get an overview of the Elimination Diet in this article. While you’re on it (and in the future), you’ll want to make sure you start each day with a savory, protein-rich breakfast.
For more guidance on diet for hormone balance, consider getting my book, Overcoming Estrogen Dominance.
It’s best if you can also reduce or (better) eliminate alcohol – such is a common social lubricant but also one that greatly contributes to inflammation.
Unfortunately, alcohol can really mess with your hormones, and it’s likely to take you longer to get a hold on inflammation and insulin levels while you’re still consuming alcohol.
For those who need to go deeper to get a handle on blood sugar, a “keto-green” diet might be a good way to go. This is a ketogenic diet that really focuses on getting plenty of green leafy vegetables, as recommended by Dr. Anna Cabeca. Reducing sugar and processed carbs while also increasing fiber intake is essential.
Exercise – Weight Training, Not Cardio
A lot of women, in their effort to get rid of belly fat, think that running is the answer. Running (or other cardio) is actually the worst thing you could do. To the body, cardio = stress, and stress = cortisol. Cortisol throws off your hormones, increases inflammation, and is one of the contributors to belly fat.
Instead, start getting to weight training or resistance training. This moves your body and strengthens muscles without putting your body into fight-or-flight. Researchers have found resistance training to both decrease belly fat and increase insulin sensitivity. (8)
Correct Hormone Levels
As long as your hormones are out of balance, it’s going to be pretty difficult to lose belly fat. That’s because…
- Estrogens
- Cortisol
- Insulin
- Glucagon
- Testosterone
- Growth hormones
- IGF-1
- Thyroid hormones
… all help regulate blood sugar control. So, if just one of those is out of balance, you’ll still have trouble balancing your blood sugar, and consequently, you’ll have trouble getting rid of the belly fat.
Correcting hormone levels and getting them balanced is essential.
Add Botanicals, Vitamins, and Minerals
There are several botanical (herbal), vitamin, and mineral supplements you can add to lower inflammation and support insulin sensitivity of the cells. We’ll start with the anti-inflammatory ones: (9)
Anti-Inflammatories
- Fish Oil: 2-3 grams, once a day
- Vitamin D3: 5000 IU once a day
- CoQ10: 60-100, mg once a day
- Magnesium glycinate: 600-1200 mg
- Selenium: 200 mcg
Insulin-Supporting
- Cinnamon: ½ teaspoon, once a day. Lowers blood sugar and increases insulin sensitivity.
- Chromium: 200-600 mcg. Increases insulin sensitivity and improves glucose control.
- Fenugreek: 750 mg capsules, twice a day.
- Apple pectin, beet powder, oat fiber: Slows glucose absorption into the bloodstream, also lowering insulin.
- Milk thistle: 200-400 mg. Lowers fasting glucose, average daily glucose, and fasting insulin levels.
- Gymnema Sylvestre: 400 mg, twice a day. Lowers blood sugar and improves insulin sensitivity. Also regenerates beta cells in the pancreas.
- Bitter melon: (10:1) 250 mg twice a day. Suppresses blood glucose spikes after sugar intake.
Microbiome-balancing
Research is now showing that microbiome correction can help change the body composition in the body. For example, in this study concluded that probiotics can change body fat mass composition. The Flat Belly Probiotic was developed based on this research.
You don’t need to take all of these. This is just a list of some compounds to research and consider. If all that seems overwhelming, here’s where to start.
Where to Start
#1 Diet
No matter what, begin by looking at your diet. If you’re constantly triggering inflammation and spiking blood sugar with what you’re eating, it’s going to be nearly impossible to lose belly fat. Doing the elimination diet is a good way to lower inflammation fast, reduce sugar intake and improve insulin sensitivity. From there, you can move on to Cooking For Hormone Balance or the meal plan in Overcoming Estrogen Dominance.
#2 Supplement Support
Supplements can support your diet and lifestyle changes. You can consider one or more of the anti-inflammatory and insulin-supporting supplements above. However, if you’d rather add in a couple of supplements that support the body synergistically, here’s what we have found that works for a lot of women:
Microbiome support:
Flat Belly Probiotic – This probiotic was formulated based on the latest research showing changes in body fat mass, reduction in food intake, and healthy weight management. It’s been a highly popular product with our Wellena / Hormones Balance community.
Blood Sugar Balance:
Gluco Maximus – This supplement helps to support healthy blood sugar and cholesterol levels. It also improves/maintains healthy nerve function. The star ingredient is CinSulin®, a cinnamon (Cinnamomum cassia) extract that is clinically proven to influence blood sugar metabolism. It helps glucose get into cells to support energy production.
Other key ingredients include American Ginseng, Gymnema Leaf Extract, Green Tea Polyphenols, and Chromium.
Estrogen-Progesterone Balance:
Wise Women’s Balance – This supplement helps improve symptoms of low estrogen and helps relieve menopausal discomfort, including hot flashes. It also supports natural aromatase activity (the conversion of testosterone to estrogens) and may help block “dirty” estrogens while raising progesterone and helping to manage estrogen dominance.
ProgestPure – this topical bioidentical progesterone helps to raise progesterone levels, helping sleep and balance the estrogen-to-progesterone ratio.
Each of these supplements and compounds mentioned above can support you in getting rid of unwanted belly fat.
Learn more with Overcoming Estrogen Dominance
“The body has an amazing ability to heal. We just need to give it the right resources.”
In Overcoming Estrogen Dominance, my goal is to empower and give you the tools to take control of your hormones and health.
More than 70% of women experience estrogen dominance. The symptoms range from lumpy and fibrocystic breasts to thyroid nodules, hot flashes, fibroids, uterine polyps, painful, heavy or irregular periods to infertility and miscarriages, from mood swings to insomnia, weight gain to fatigue.
So many women have experienced the pain and frustration that comes when they feel their symptoms and complaints are dismissed or minimized. This is particularly true for women who are experiencing the symptoms of hormone imbalance. Even when doctors do offer treatment, it’s typically in the form of prescription medication or invasive surgical procedures.
In Overcoming Estrogen Dominance, I hope to show that those extreme interventions are often unnecessary, and to give women a roadmap to reverse estrogen dominance using food, herbs, supplements and natural protocols to rebalance hormones.
To get your copy of Overcoming Estrogen Dominance, go here.
Resources
- Harvard Health Publications. “Abdominal fat and what to do about it.” Harvard Health Publishing. 2019.
- Wszelaki, Magdalena. Overcoming Estrogen Dominance. Hormones and Balance. 2021.
- Shou, J., Chen, PJ. & Xiao, WH. Mechanism of increased risk of insulin resistance in aging skeletal muscle. Diabetol Metab Syndrome. 2020.
- Ariaans, G et al. “Cancer-drug induced insulin resistance: innocent bystander or unusual suspect.” Cancer treatment reviews. 2015.
- Jeremy, R, and H Davies. “Monomer complexes of polyadenylic acid.” Biochemical Society transactions. 1975.
- Wang, Yue-Hao et al. “Human cytochrome p450c17: single step purification and phosphorylation of serine 258 by protein kinase a. Endocrinology. 2010.
- Wadden, Thomas A et al. “Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy.” Circulation. 2012.
- Westcott, Wayne L. “Resistance training is medicine: effects of strength training on health.” Current sports medicine reports vol. 11,4 (2012): 209-16. doi:10.1249/JSR.0b013e31825dabb8
- Lommen, Erin. “Belly Fat and High Androgens in Women; Advancing your clinical success with Insulin Resistance, Metabolic Syndrome, and PCOS. Labrix Clinical Services, Inc. 2013.

Much obliged to you for sharing your experience, I will utilize your recommendation. I’m effectively chipping away at getting thinner, and my better half, going against the norm, is dealing with acquiring bulk. He was exhorted and the outcome was not long in coming.
Im going to try this
Thank you for all the information! Couple of questions:
1. Does swimming (cardio, but low impact) register as stress—> increased cortisol?
2. Does increasing protein – somewhat unrelated to carb intake – improve insulin resistance? Heard a bioscientist say they thought (but have not confirmed via study review), weight loss, at least, on this diet might have more to do with increased protein (versus reduced carbs)..
Appreciate a response on this website (I give a fictitious email address to minimize future unwanted marketing)
Thanks!
I had cancer and had a full hysterectomy at age 38. I am 51. I cannot take Estrogen due to a stroke I had just before the cancer. I am very conscious of what I eat, not only for myself, but for my 4 grandchildren. I have Rheumatoid Arthritis, Fibromyalgia, Neuropathy, and have always been Hypoglycemic. This last year has been constant weight gain, partially to stress from my mom’s passing. I would appreciate any information you can help me with to get a handle on this belly fat.
Thank You
I’m 52 and I’m on biodentical hormones since my hysterectomy can I use these supplements? I have belly fat and definitely some extra weight in my hips and thighs.I sleep amazing. I workout everyday but I have a lot is stress in my life .
Do you think another contributing factor to consider is reducing chronic stress/fight flight from unresolved trauma? Ultimately, if those things aren’t healed or managed, I could implement all the diet/lifestyle changes and it won’t matter because my cortisol is consistently high, thus, contributing to the hormone imbalance. I understand this won’t apply to everyone but I do think constant stress in our modern world is something to consider in general.
I’m going to give this a try.
I would encourage everyone working on this issue to include some form of work on the mind’s subconscious patterns, too (hypnotherapy is one approach), as prolonged resistance to change may arise not only from the physical, but also on the energetic level, where many physical issues have their origins. Neville Goddard’s books, although the language is now somewhat “quaint,” remain an excellent guide to learning to focus on/co-create what we want, versus being stuck in the cycle of bemoaning the persistence of what we don’t want (“energy flows where attention goes”).
I need some advice on being 75 and starting to see frizzy hair, wrinkles and sagging everywhere! lol it’s like it’s all heading to the floor!!! I am very naturally minded so I am careful what I put on my skin and in my body. Would progesterone help this at all?