What you will learn
- Perimenopause is the most normal phase in a woman’s life
- What’s going on in your body?
- What are the symptoms of perimenopause?
- What lab tests can confirm perimenopause?
- How to prepare for menopause?
- Perimenopause isn’t just one hormonal imbalance
- Perimenopause and low estrogen levels
- Perimenopause and low progesterone levels
- Perimenopause and estrogen dominance
- Perimenopause and blood sugar levels
- Perimenopause and cortisol How to prioritize your treatment plan
Perimenopause is the most normal phase in a woman’s life
For many women including me, heading into perimenopause and menopause felt like a distant and abstract concept – which I intellectually understood but didn’t feel and experience.
Until summer 2022 – it really hit me.
Hot flashes, onset of some incontinence when jumping rope (yes, that is the #1 most embarrassing one because it happened at a gym), receding gums, shorter cycles, less bleeds. Clearly, something has started shifting and I had to stop the denial.
Entering menopause is a lot more clear-cut – having no period for 12 months, elevated FSH/LH (more on that below) is pretty much it. But perimenopause? There are no clear guidelines on what to look for. You’re still cycling but things just aren’t the same.
Because of that, we look for external reasons why strange health issues have crept in – blaming it on our partner, job, too much wine, or the weather. When that’s not working, we start getting angry and surprised with our body, as if it started betraying us.
The truth is: it might be perimenopause.
I feel like there are no solid resources to support women in perimenopause (menopause has gotten a little more limelight as of late) – this is why we decided to dedicate a lot more resources to talking about it.
Here are some of the earliest symptoms of perimenopause:
- Shorter cycles (by 2 to 7 days)
- Less bleeding days (by 1 to 3 days)
- Periods start being irregular and unpredictable
- Your PMS is worse than ever (what?!)
- Your breast pain is worse You don’t sleep well anymore
- You got your first hot flash! (feel that furnace in your abdomen?)
- Incontinence happened once or twice
- You got a UTI out of nowhere
What’s going on in your body?
Hot flashes, shorter periods, and worse PMS are often the first symptoms of entering perimenopause.
Women who had bad PMS as a young woman tend to have worse perimenopause – but that can be changed.
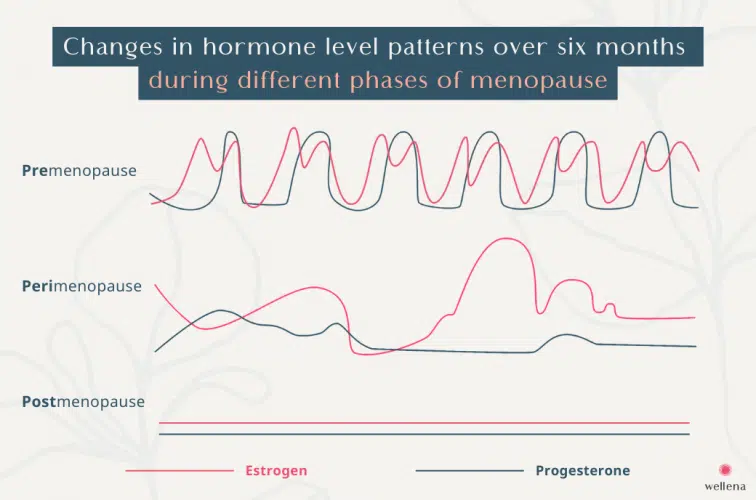
The biggest hormonal change that happens are dropping estrogen and progesterone levels. It’s not a straight line, however. It can be chaotic, irregular, surprising, and unpredictable.
So what’s going on?
Hormonal fluctuations: As we age, our ovaries produce fewer hormones, leading to irregularities in the menstrual cycle. Estrogen levels may fluctuate greatly, causing changes in the timing and duration of periods. These hormonal shifts can have a wide range of effects on the body and can impact mood, energy levels, and other bodily functions. The ovaries try to keep up with the old production schedule but now more often than not, they simply can’t – and this can cause drastic and unpredictable cycle changes.
One thing in Perimenopause is certain – nothing feels “normal” anymore.
Ovarian follicle depletion: With age, the number and quality of eggs in the ovaries decrease. This can result in irregular ovulation or the absence of ovulation altogether. Consequently, hormone levels can become imbalanced causing FSH and LH to increase. Some women in perimenopause experience ovulatory pain at random times of the cycle.
Decline in estrogen: Estrogen is a key hormone that regulates many aspects of a woman’s reproductive system. Its decline during perimenopause affects multiple areas, such as the uterus, brain, vagina, and breasts. These changes can lead to symptoms such as vaginal dryness, reduced elasticity, forgetfulness, and changes in breast tissue.
Changes in the menstrual cycle: Perimenopause is characterized by irregular periods, where the cycle length may vary, and bleeding may be heavier or lighter than usual, or both. These changes occur due to hormonal fluctuations and the ovaries’ reduced ability to release eggs consistently.
Physical and emotional symptoms: Hormonal changes during perimenopause can impact a woman’s physical and emotional wellbeing. Common symptoms include hot flashes, night sweats, mood swings, sleep disturbances, fatigue, irritability, anxiety, and depression. These changes can vary in intensity and duration among individuals.
I want to reiterate that while perimenopause is a natural phase of a woman’s life, the symptoms experienced can be challenging and for some women, debilitating. Our community regularly reports cases of lost jobs, end of relationships, loss of confidence, and inability to pursue passions and activities loved in the past.
This is what brought this long article together. My mission is to normalize this phase of your life and empower with options of natural interventions and self-help.
What are the symptoms of perimenopause?
The earliest symptoms of perimenopause include:
- shorter cycle (by 3-5 days)
- shorter bleed days
- lighter or heavier bleed days (compared to before)
- mid-cycle spotting
- lack of ovulation
- hot flashes
- incontinence
- mood swings
- breast changes (pain, swelling, benign cysts)
If you experience two or more, you most likely entered perimenopause.
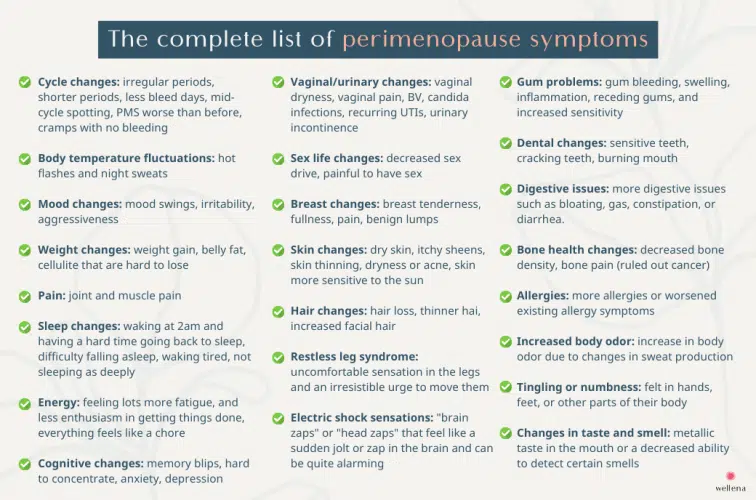
Here is the complete list of perimenopause symptoms:
- Cycle changes: irregular periods, shorter periods, fewer bleed days, mid-cycle spotting, PMS worse than before, cramps with no bleeding
- Body temperature fluctuations: hot flashes and night sweats
- Mood changes: mood swings, irritability, aggressiveness
- Weight changes: weight gain, belly fat, cellulite that are hard to lose
- Sleep changes: waking at 2am and having a hard time going back to sleep, difficulty falling asleep, waking tired, not sleeping as deeply
- Energy: feeling lots more fatigue, and less enthusiasm in getting things done, everything feels like a chore
- Cognitive changes: memory blips, hard to concentrate, anxiety, depression
- Vaginal/urinary changes: vaginal dryness, vaginal pain, BV, candida infections, recurring UTIs, urinary incontinence
- Sex life changes: decreased sex drive, painful to have sex
- Pain: joint and muscle pain
- Breast changes: breast tenderness, fullness, pain, benign lumps
- Skin changes: dry skin, itchy sheens, skin thinning, dryness or acne, skin more sensitive to the sun
- Hair changes: hair loss, thinner hai, increased facial hair
- Bone health changes: decreased bone density, bone pain (ruled out cancer)
- Electric shock sensations: “brain zaps” or “head zaps” that feel like a sudden jolt or zap in the brain and can be quite alarming
- Tingling or numbness: felt in hands, feet, or other parts of their body
- Gum problems: gum bleeding, swelling, inflammation, receding gums, and increased sensitivity
- Dental changes: sensitive teeth, cracking teeth, burning mouth
- Digestive issues: more digestive issues such as bloating, gas, constipation, or diarrhea.
- Allergies: more allergies or worsened existing allergy symptoms
- Increased body odor: increase in body odor due to changes in sweat production
- Changes in taste and smell: metallic taste in the mouth or a decreased ability to detect certain smells
- Restless leg syndrome: uncomfortable sensation in the legs and an irresistible urge to move them
A long list, huh?
If you experience two or more, you most likely entered perimenopause. If you’re ticking 3 or more, you most likely are having a hard time going through it.
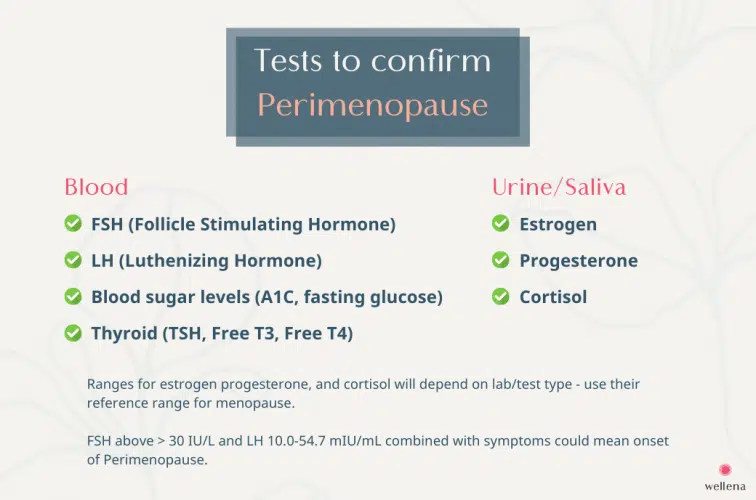
What lab tests can confirm perimenopause?
Hormones such as estrogen, progesterone, and cortisol are steroid hormones best measured in urine or saliva, not blood. Blood (serum) testing is highly reliable but for blood sugar levels, FSH, LH, and thyroid hormones (and many other things), not steroid hormones.
How and where to test estrogen, progesterone, and cortisol levels?
DUTCH test (urine) is the golden standard for estrogen levels, estrogen metabolites (to understand the metabolism of the “dirty” estrogens and estrogen dominance), progesterone, cortisol, DHEA, and testosterone levels. You can order the labs on your own and get a discount for our community here.
Saliva testing is great for understanding the various estrogen levels, progesterone, cortisol levels (it doesn’t measure estrogen metabolism though, to determine the level of “dirty” estrogens). You can self-order on the Canary Club website.
How and where to test blood sugar levels, thyroid, FSH, and LH?
Blood (serum) testing is great for sugar levels, thyroid, FSH, and LH; and most physicians, even the conventionally-trained, conservative ones, should be able to order them for you. If not, change your physician to one who is open-minded and ready to support you. Tests to confirm perimenopause are:
- FSH (Follicle Stimulating Hormone) – FSH is released by the pituitary gland to stimulate the ovaries to produce more estrogen and progesterone. During menopause, FSH levels typically rise, so a high FSH level, especially when combined with menopausal symptoms, can suggest menopause. FSH levels of > 30 IU/L, combined with an onset of the above-mentioned symptoms could mean the start of perimenopause.
- LH (Luteinizing Hormone) – LH is also released by the pituitary gland as a chemical agitator that spurs your reproductive system to action and release estrogen, progesterone, testosterone. When we enter perimenopause, LH tends to rise and fall into the range of 10.0-54.7 mIU/mL.
Auxiliary blood tests to order if you suspect thyroid issues (common in perimenopause):
- TSH
- Free T3 (not total)
- Free T4 (not total)
- TPO antibodies (to rule out Hashimoto’s)
- anti-TG antibodies (to rule out Hashimoto’s)
How to prepare for perimenopause?
A detailed plan of action will depend on what kind of perimenopause you experience (depending on which hormonal imbalances drive it) – we go into details below.
However, there are 5 key changes you can make today to lay a strong foundation to sail through perimenopause. These changes can and should be made regardless of which hormonal imbalance(s) you experience while going through perimenopause.
- Diet
- Fixing mineral deficiencies
- Adding a few herbs
- Getting quality sleep and rest
- Less stress
#1 Diet
A well-balanced, nutrient-dense, and anti-inflammatory diet plays a crucial role in supporting women during perimenopause. You can’t out-supplement your diet. Avoiding gluten, dairy, processed foods, and excessive sugar are key. Foods rich in phytoestrogens, such as soy (organic, unprocessed), flaxseeds, and lentils, can help regulate estrogen levels and alleviate symptoms like hot flashes and mood swings. Incorporating plenty of fruits and green vegetables ensures an adequate intake of vitamins, minerals, and antioxidants, supporting overall health. A specific group of vegetables called “crucifers” have a special affinity for the liver, an organ vastly underestimated when it comes to hormonal health in women. Additionally, consuming omega-3 fatty acids found in fatty fish like wild salmon or taking supplements can reduce inflammation and promote hormonal balance.
Solution: Check out our blog recipes or get one of our books: Overcoming Estrogen Dominance (I’ve found that estrogen dominance is the leading hormonal imbalance making perimenopause worse) and Cooking for Hormone Balance.
#2 Common vitamin and mineral deficiencies
Several minerals are essential for hormone regulation, and deficiencies can exacerbate perimenopausal symptoms. Vitamin D3 is key in production and metabolism of estrogen and progesterone. B vitamins are essential in liver health and hormone metabolism. Magnesium supports liver health, bone density, aids in managing mood swings and sleep disturbances. Iron deficiency can worsen fatigue, a common symptom during this phase. Zinc is necessary for hormone synthesis and can contribute to overall hormonal balance. Ensuring adequate intake of these minerals through diet or supplementation is important for women in perimenopause.
Solution: We carry a number of above in our store – Wellena.com.
#3 Herbs
Certain herbs have been traditionally used to alleviate perimenopausal symptoms. Black cohosh is a popular herb known for its potential to reduce hot flashes and improve sleep quality. Dong quai is another herb that may help regulate hormone levels and reduce menstrual irregularities. Gamma-linolenic acid (GLA) found in borage seed oil or evening primrose oil may alleviate breast pain and tenderness; and reduce PMS. Vitex (aka chasteberry) can increase progesterone levels. Maca is believed to have adaptogenic properties, meaning it helps the body adapt to stress and normalize hormone levels.
Solution: Check out our Wise Women’s Balance herbal formula containing a number of the above herbs. Got your favorite ones? Start taking them.
#4 Sleep and rest
It can be frustrating to hear it – prioritizing sleep when you can’t sleep out of the sudden. One of the reasons for poor quality of sleep in perimenopause is dropping progesterone and/or estrogen levels. Quality sleep and sufficient rest are vital for women going through perimenopause.
Solution: There is a lot you can do to help yourself. I’ve written a long article about sleep (that took me 8 months to compile) – go down the list and see what your causes could be.
#5 Less stress (reduce high cortisol levels)
Chronic stress can negatively impact hormonal balance and exacerbate perimenopausal symptoms. High cortisol levels, often associated with stress, can lead to increased inflammation, anxiety, mood swings, and disrupted sleep patterns. Engaging in stress-reducing activities like regular exercise, practicing mindfulness or yoga, and engaging in hobbies or activities that bring joy can help manage stress levels. Prioritizing self-care, setting boundaries, and seeking support from loved ones or professional counselors can also contribute to a healthier emotional state during perimenopause. By actively managing stress, women can improve their overall well-being during this phase of life.
Perimenopause isn’t just one hormonal imbalance
Perimenopause isn’t just one hormonal imbalance as it gets brought on by various hormonal changes including dropping estrogen and progesterone, estrogen dominance, imbalanced cortisol levels, and fluctuating blood sugar levels.
The rest of the article will walk you through each hormonal imbalance. Understanding which ones might need your attention will help you create an action plan – and when you implement it, symptoms will lessen.
Let’s dive into each one of them.
Perimenopause and low estrogen levels
As our ovaries start to retire, we produce less estrogen. Dropping estrogen levels is one of the earliest symptoms of perimenopause.
What are the symptoms of low estrogen?
- Irregular or absent menstrual periods
- Hot flashes and night sweats
- Vaginal dryness and discomfort
- Incontinence, frequent UTIs
- Mood changes and sleep disturbances
- Fatigue and decreased energy
- Changes in bone health and density
- Cognitive changes; difficulty with memory, concentration, focus, and “brain fog”
- Sleep quality: lack of deep and REM sleep, frequent waking, getting up feeling tired
- Muscle weakness, sagging skin
How does it impact perimenopause?
As you can see from the above symptoms, many of them impact how you experience perimenopause. Resolving them might help you feel better in this part of your life.
What can you do?
A lot. Correcting estrogen levels can drastically improve the symptoms of perimenopause.
If you experience many of the above symptoms, consider getting Cooking for Hormone Balance and follow the menopause protocol.
We also created a supplement that helps to raise estrogen levels using botanicals that contain gentle phytoestrogens (Black Cohosh, Hops, Norwegian spruce), vitamins (B6, B12) and minerals (calcium d-glucarate, magnesium) called Wise Women’s Balance.
This blend of vitamins, minerals, and botanical extracts is designed to support healthy estrogen levels and natural estrogen detoxification during menstruation and through menopause. It contains a synergistic blend of nutrients designed to aid the body’s natural hormonal balance.
What could help as well
Botanical options
Estrogen Boost supports healthy estrogen levels and may relieve normal perimenopausal discomfort. This formula delivers a unique, proprietary blend of 8-prenylnaringenin (8-PN) from hops and plant-lignin extract at clinically relevant levels to correct estrogen levels.
Magnesium Replenish optimizing magnesium levels supports the endocrine system on many levels; from facilitating better sleep, regular bowel movement, to supporting liver detoxification.
Bioidentical hormone replacement option
If you prefer to use exogenous estrogen, we recommend bioidentical, topical version, not oral. We currently don’t offer one but you could check out BioLabs product collection.
Perimenopause and low progesterone levels
What is it?
Progesterone is at its highest in our reproductive years. The hormone name means pro-gestation. Naturally, it will start dropping as our ovulation winds down together, and we no longer produce as many eggs and the corpus luteum – which produces progesterone.
What are the symptoms?
- Irregular menstrual cycles
- Heavy or prolonged menstrual bleeding
- Mood swings and irritability
- Anxiety or increased feelings of stress
- Insomnia or disrupted sleep patterns
- Breast tenderness or swelling
- Changes in libido or decreased sex drive
- Fatigue or low energy levels
- Difficulty with concentration or memory
- Water retention or bloating
- Hot flashes and night sweats
- History of miscarriages
How does it impact perimenopause?
Correcting progesterone levels could improve your overall perimenopause experience, especially if you are ticking many of the above boxes.
What can you do?
You can correct progesterone levels by either using botanicals or bioidentical topical progesterone.
Vitex (aka Chasteberry) is a revered herb (well studied and used by mainstream medicine in many European countries) that can raise progesterone levels. Check out our Chasteberry supplement.
If you prefer a topical solution, we carry a cream and an oil in our store. Both are made from yams, and are very clean (contain no phthalates, mineral oils, synthetic fragrances, toxic preservatives or emulsifiers). Check out the ProgestPure Cream.
Perimenopause and estrogen dominance
What is it?
It’s a hormonal imbalance that women in perimenopause very often experience. It may sound incorrect and illogical to be “dominant” in estrogen when our hormones start dropping.
Let me explain. Estrogen dominance can happen in two main situations:
- When your estrogen-to-progesterone ratio is off (we call it Type 1 Estrogen Dominance) – with typically too much estradiol and too little progesterone to oppose it.
- When you break down estrogens to too many “dirty” ones (which happens in the liver and the GI tract)
What are the symptoms?
CYCLE CHANGES
- Mid-cycle spotting
- Heavy periods
- Scanty periods
- Irregular periods
INFLAMMATORY
- Hot flashes
- Allergies
- Autoimmune diseases
UTERINE CHANGES
- Fibroids
- Uterine polyps
EXTERNAL CHANGES
- Hair loss
- Spider or varicose veins
- Bloating, puffiness or water retention
- Cellulite
- Stubborn butt and thigh fat
- Melasma (brown skin pigmentation)
BREAST CHANGES
- Fibrocystic breasts
- Breast cysts
- Enlarged, swollen, tender breasts
COGNITION & MOOD
- Brain fog
- Depression
- Irritability
- Mood swings
- Anxiety
- Headaches or migraines, particularly before the period
SLEEP
- Trouble falling asleep
- Trouble staying asleep
- Reduced deep sleep
DIGESTION
- Gallstones, gallbladder problems/removal
SEXUALITY & FERTILITY
- Low libido
HORMONAL CHANGES
- Low thyroid function
- High blood sugar levels
- Insulin resistance
CANCERS & NODULES
- Breast (ER+ or PR+) cancer
- Ovarian cancer
- Uterine cancer
- Lung cancer
- Thyroid cancer
- Thyroid nodules
How does it impact perimenopause?
In a big way! Just see above how many of the symptoms you might also be experiencing in perimenopause. Resolving them might help you feel better in perimenopause.
What can you do?
A lot. This is the biggest hormonal imbalance I’ve personally struggled with. I even wrote a book about it.
If you experience many of the above symptoms, consider getting Overcoming Estrogen Dominance.
We also created a supplement kit that helps to metabolize estrogens (less of the “dirty” ones and more of the “good” ones) – it’s called the Estrogen Reset Kit. (When you get the kit, you save $18.90.)
Perimenopause and high/low cortisol
What is it?
Got stress? Emotional, physical, spiritual, or chemical? If you’re a normal human being, you’ve probably experienced these or maybe still do. During times of stress, the body releases additional levels of cortisol for the body to cope. This could be problematic due to elevated inflammation and reduction of progesterone levels – leading to a cascade of hormonal imbalances.
How does it impact perimenopause?
In a big way. The adrenals are even more precious during perimenopause because they partly take over estrogen production from the ovaries. As we age, our ovaries slow down and reduce estrogen output – this is when the adrenal glands pick up. Well-functioning adrenals can make perimenopause an easier experience.
What are the symptoms?
Overstimulated adrenal health (high cortisol) has symptoms such as:
- Tired and wired
- Trouble sleeping
- Midnight waking
- No energy in the morning
- Can’t fall asleep
- Belly fat
- Anxiety
- Short fuse
- Coffee cravings
- Hair loss
- Understimulated adrenal health (low cortisol levels) can manifest as these symptoms:
- Severe fatigue
- Memory loss
- Frequent sickness
- Overreacting
- Crying spells
- Lack of motivation
- Lightheadedness
- Salt cravings
- Low sex drive
- Unstable blood sugar levels
Can you experience both?
Yes. There may be days or times of the day when the adrenals go either way. Many women experience underactive adrenals in the morning (need 2 cups of coffee to “wake up”) and overactive adrenals at night (can’t fall asleep, feel “wired but tired”).
What can you do?
- Ask yourself what are the sources of your stress and how can you reduce and eliminate them? (Stress can be emotional, physical, spiritual, or chemical.)
- Prioritize sleep and day rest (it’s not laziness).
- Get on an anti-inflammatory diet (both our cookbooks use this approach; Cooking for Hormone Balance and Overcoming Estrogen Dominance)
- Reduce or stop coffee and alcohol. Yes, we know it’s tough but so, so worth it.
- Consider adding adaptogens (botanicals that help regulate the HPA axis). These include Rhodiola, Asian ginseng, Tulsi (Holy Basil), Cordyceps, Licorice (best for underactive cases). Our Adrenal TLC has been formulated with many of these.
- In times of stress, the body uses excessive amounts of vitamins C, B (especially B5 and B6), and magnesium. Adding supplements during stressful times or during recovery is highly recommended. We carry Magnesium Replenish, B Maximus, and Vitamin C Complete (100% food-derived) if you want to check it out.
If your condition is chronic, consider working with a functional practitioner.
Perimenopause and blood sugar levels
What is it?
As we age, it’s normal for our blood sugar levels to fluctuate and often be higher than in our younger days. Many women in perimenopause experience high blood sugar levels and even develop pre-diabetes or diabetes. With age, our insulin receptors aren’t as responsive to insulin (which sweeps up the glucose from the blood and brings it into the cells) – and this can result in high blood sugar levels.
How does it impact perimenopause?
High blood sugar levels will increase inflammation, tax out the adrenals (cortisol also helps to regular blood sugar levels, not just stress), cause hot flashes, and weight gain (especially the belly).
What are the symptoms?
- Hot flashes and night sweats
- Mood swings and irritability, especially when hungry
- Anxiety and lack of grounding, especially when hungry
- Hunger after a meal
- Frequent urination
- Blurred vision
- Fatigue and energy fluctuations
- Weight gain and difficulty losing weight (especially around the abdomen)
- Brain fog and cognitive issues
- Increased risk of chronic conditions
- Numbness or tingling in the feet or hands
- Frequent infections
- Slow-healing sores
- Blood work that shows glucose levels above 90 mg/dL
- Blood work that shows HA1C level above 5.4%
What can you do?
A lot! Here are a few simple action items you can start tomorrow.
- Breakfast – Start your day with a savory breakfast that predominantly consists of protein, fat, and fiber. (Oatmeal, fruit smoothies, and even protein shakes will increase your blood sugar levels.) Both our cookbooks Overcoming Estrogen Dominance and Cooking for Hormone Balance have many savory breakfast ideas.
- Sugar count – You may be surprised how much sugar you consume on a daily basis. For one or two days, count how much sugar is in all the food and drinks you consume. Include store-bought soups, ketchups, iced tea, latte, and fruit. For healthy blood sugar levels and balanced hormones, your daily intake should be no more than 20 grams of sugar.
- Add botanicals and minerals – herbs such as cinnamon, gymnema, fenugreek, kudzu help lower glucose levels and re-sensitive insulin receptors. Trace minerals such as chromium have an excellent profile in supporting healthy glucose metabolism and enhancing insulin action. Consider getting our Gluco Maximus which contains many of the mentioned botanicals and minerals.
How to prioritize
The common question we get is – I’m most likely in Perimenopause and I have so many of the above symptoms – where do I start? How do I prioritize my action plan?
There are a few things you could do:
- Work with a skilled functional practitioner such as a functional/integrative/holistic physician, naturopath, nurse practitioner, or health coach who specializes in women’s hormonal health. The last part is important – hormones are a speciality area and few practitioners are truly skilled in this area. You can find practitioners by searching online or checking out this directory. Your practitioner should be able to help you create and prioritize the treatment plan. Options that should be discussed are urine/saliva/blood testing, diet changes, supplements, herbs, bioidentical hormones, sleep, meditation, and detoxification at the very least.
- If you decide to DIY it, we recommend to:
- Use the above symptoms lists to determine which hormone imbalances you may experience to the largest degree. Start there.
- If you’re experiencing many symptoms in each (such as low estrogen, cortisol issues, low progesterone), start with stabilizing your cortisol levels first. Your HPA axis/adrenals can have a big impact on the rest of your hormones – so start there.
- Based on your symptoms, we provided herbal and supplement options for you to choose from – but remember that diet, sleep, and rest will be foundational to transitioning into Perimenopause. Don’t marginalize or neglect them.
I know this is a long and dense article. Oversimplifying it won’t have been helpful – so save it, print it, re-read it and let it sink in. What I want you to take away from it is that: Perimenopause is a given, but going through hell is optional.
If you need support, our Customer Experience team is here to help you – just contact us through our contact form.

Thank you for all of this- I was starting to feel crazy b/c last Nov 2022 at 49 1/2 years old, I developed pretty severe joint/muscle pain despite working out every day. I am very active but this was awful. It was like a light switch. Anyway, I’ve been to two different orthopedics and a chiropractor and have no arthritis. I even had platelets injected into knees, nothing has helped. But I appreciate your article and am going to read it over and over again.
Check your Testosterone levels, pain might be due to low Testosterone. Been there.
I agree with the comment about Testosterone. Mine had tanked and I was having really bad joint pain. Been on a Testosterone cream for over a year and the relief is tremendous. Find a gynecologist or someone who specializes in Menopause. Also the Reddit thread r/menopause is filled with women going through it and so much support.